Two years on, Ayushman Bharat has ground to cover on universal health care
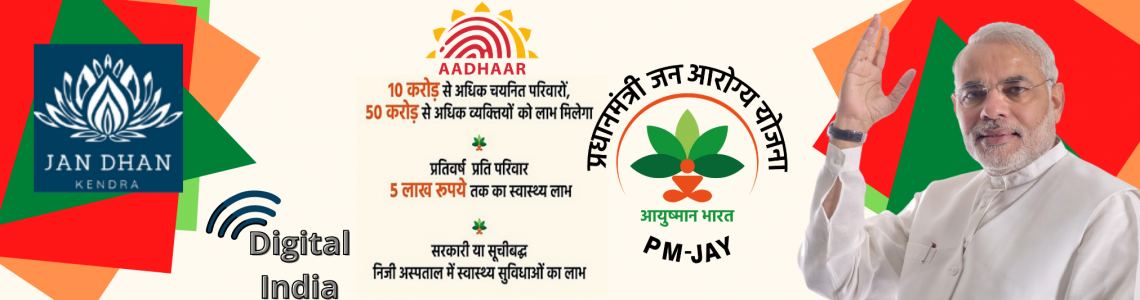
The Centre’s flagship Ayushman Bharat health insurance programme has completed two years. But this time, the buzz around the milestone has been low-key, coming at a time when hospitals are coping with the surge in Covid-19 numbers.
Launched on September 23, 2018, in Ranchi, the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana has seen over 1.26 crore hospitalisations, involving a spend of over ₹15,772 crore to cover these healthcare bills. In fact, Health Minister Dr Harsh Vardhan said the two-year milestone is as significant as his involvement with polio eradication efforts in the country.
The National Health Authority’s Chief Executive Dr Indu Bhushan said, at an event to herald the two-year milestone, over 23,311 hospitals were on board the scheme covering over 1,500 procedures. The scheme has generated savings to the tune of ₹30,000 crore, he said.
But the scheme still has ground to cover in terms of being more universal in its coverage, say public health voices, even as private healthcare representatives seek greater dialogue to “iron out the wrinkles”.
Exclusion
Making a case for universal healthcare, KM Gopakumar with the Third World Network, points out that a bulk of the middle class remains outside the scheme. And the “package system”, where a set number of procedures are covered for reimbursement by the government, leads to further exclusion of ailments and people, he said.
The scheme is the first step towards providing universal healthcare, said Dr Sudarshan Ballal, Chairman, Manipal Health Enterprises. “Not just the Western nations, but even countries such as Thailand have a well-developed healthcare system,” said Dr Ballal, who is also a former president of NATHEALTH, a platform for hospitals, diagnostics, insurance providers etc.
The last six-odd months have been low-key, he admits, as all efforts have been redirected to tackling Covid. But the effort now should be to dialogue with private providers, address their viability problems and encourage more low-cost or no-frills hospitals, upscaling of teaching hospitals, and even private-private partnerships like the one Manipal Health has with the Tata’s hospital in Jamshedpur for clinical training, he said.
Private players ask for more support
In the early days of the scheme, the pricing of procedures had been a major bone of contention for private healthcare providers, including smaller nursing homes run by medical professionals. In fact, Ballal says, large corporate hospitals are still not entirely participating in the scheme for these reasons.
Lauding the concept of wellness centres, he said there should be attention on prevention and greater screening at the primary centres before a patient lands up at a tertiary care hospital. Hospitals will be willing to get more involved if there was a viability-gap funding mechanism to help hospitals support low-cost procedures. Other alternatives that private healthcare providers have been suggesting to the government include a differential pricing of sorts to support cross-subsidisation of those who cannot pay, by those who can.
Patient woes
Patient experiences, though, include difficulties in getting covered when there are repeated procedures, for instance, as in a chemotherapy that has multiple cycles; or when they travel to a different State for treatment. Presently, Odisha, West Bengal and Telangana are not part of the scheme. These are some of the ground realities the scheme will have to fix, so it can deliver the benefit it sets out to provide.

2089 Comment(s)
sasa
Thanks for every other informative site. The place else may just I get that kind of information written in such an ideal means? I have a venture that I’m just now operating on, and I have been on the look out for such information.
Hello There. I found your blog using msn. This is an extremely well written article. I will be sure to bookmark it and return to read more of your useful information. Thanks for the post. I’ll certainly comeback.
This is very interesting content! I have thoroughly enjoyed reading your points and have come to the conclusion that you are right about many of them. You are great.
Is it okay to post part of this on my website basically post a hyperlink to this webpage?
Your music is amazing. You have some very talented artists. I wish you the best of success.
It is imperative that we read blog post very carefully. I am already done it and find that this post is really amazing.
Wow i can say that this is another great article as expected of this blog.Bookmarked this site..
Document thrilled along with the researching you will designed to makes precise put up impressive. Delightful adventure!
I simply reckoned it is an outline to share in case other companies was first experiencing difficulty looking for still Now i'm a small amount of doubting generally if i here's permitted to use artists and additionally explains relating to right.
With thanks to get furnishing recently available posts in connection with the dilemma, I actually look ahead to learn extra.
Absolutely fantastic posting! Lots of useful information and inspiration, both of which we all need!Relay appreciate your work.
This is really a nice and informative, containing all information and also has a great impact on the new technology. Thanks for sharing it
i read a lot of stuff and i found that the way of writing to clearifing that exactly want to say was very good so i am impressed and ilike to come again in future..
Wonderful article, thanks for putting this together! This is obviously one great post. Thanks for the valuable information and insights you have so provided here.
Really special blog post, Thanks for your time designed for writing It education. Outstandingly drafted guide, if only every webmasters marketed the exact same a better standard of subject matter whilst you, cyberspace was obviously a better set. Satisfy continue the good work!
I think this is an informative post and it is very useful and knowledgeable. therefore, I would like to thank you for the efforts you have made in writing this article.
Decent Blog post, My group is a good believer on advertisment observations at online sites to help you allow web log people know they’ve applied a product favorable to help you the online world!
I've lately began the weblog, the data a person supply on this website offers assisted me personally significantly. Many thanks with regard to all your period & function.
thank you for your interesting infomation.
Thank you regarding offering latest revisions about the problem, My partner and i enjoy examine a lot more.
This was really an interesting topic and I kinda agree with what you have mentioned here!
Please continue this great work and I look forward to more of your awesome blog posts.
Thank you for taking the time to publish this information very useful!
This is a great inspiring article.I am pretty much pleased with your good work.You put really very helpful information...
This is a great inspiring article.I am pretty much pleased with your good work.You put really very helpful information...
This type of message always inspiring and I prefer to read quality content, so happy to find good place to many here in the post, the writing is just great, thanks for the post.
Thank you very much for this useful article. I like it.
Interesting post. I Have Been wondering about this issue, so thanks for posting. Pretty cool post.It 's really very nice and Useful post.Thanks
I like this post,And I guess that they having fun to read this post,they shall take a good site to make a information,thanks for sharing it to me.
It proved to be Very helpful to me and I am sure to all the commentators here!
Thank you for the update, very nice site..
This is my first time i visit here. I found so many interesting stuff in your blog especially its discussion. From the tons of comments on your articles, I guess I am not the only one having all the enjoyment here! keep up the good work
Someone Sometimes with visits your blog regularly and recommended it in my experience to read as well. The way of writing is excellent and also the content is top-notch. Thanks for that insight you provide the readers!
I think that thanks for the valuabe information and insights you have so provided here.
Love what you're doing here guys, keep it up!..
May possibly fairly recently up and running an important web log, the data one offer you on this web site contains given a hand to all of us substantially. Bless you designed for your current precious time & get the job done.
This really which means delightful not to mention original. I just absolutely adore typically the styles not to mention anyone who will become it again in your mailing could be cheerful.
Thanks for sharing nice information with us. i like your post and all you share with us is uptodate and quite informative, i would like to bookmark the page so i can come here again to read you, as you have done a wonderful job.
Thanks you very much for sharing these links. Will definitely check this out..
Positive site, where did u come up with the information on this posting? I'm pleased I discovered it though, ill be checking back soon to find out what additional posts you include.
These are some great tools that i definitely use for SEO work. This is a great list to use in the future..
I can see that you are an expert at your field! I am launching a website soon, and your information will be very useful for me.. Thanks for all your help and wishing you all the success in your business.
Really special blog post, Thanks for your time designed for writing It education. Outstandingly drafted guide, if only every webmasters marketed the exact same a better standard of subject matter whilst you, cyberspace was obviously a better set. Satisfy continue the good work!
If you're into sports betting, 토토사이트 is definitely worth checking out.
All the info I need is right there on 오피가이드 이야기
The 오피 booking system is smoother than any app I’ve tried
I found my favorite massage shop thanks to 오피가이드
Thanks, that was a really cool read!
티비위키 has every drama I love
Thanks to 오피가이드, I found a trusted massage site nearby.
Essentially I actually learn them a short while ago nonetheless I had put together quite a few opinions regarding this now Needed to read simple things them just as before for the reason that it is well crafted.
I always check op사이트 순위 before booking any massage service
탑걸주소 connects me with a community passionate about Japanese media.
Reduce financial stress using 카드 현금화.
Wonderful posting, Thanks a ton to get spreading The following awareness. Wonderfully authored posting, doubts all of blog owners available precisely the same a higher standard subject material just like you, online has got to be improved site. I highly recommend you stay the best!
클라우드 기반 링크모음으로 여러 기기에서 동시에 접근하는 게 좋아요.
Them believes magnificent to read simple things these enlightening plus exceptional reports against your web pages.
Regards for the purpose of post this amazing piece of writing! I recently came across yuor web blog perfect for your preferences. It includes marvelous not to mention advantageous items. Cultivate monetary management give good results!
In reality That i look over it all not long ago however , I saw it certain thinkings about that and after this I want to read the paper it all for a second time given that it's well written.
SR Risk Management Private Investigator certified in various types of private investigation in Malaysia like matrimonial, infidelity, matrimony detective.
오피스타 helped my company reduce overhead costs on office supplies.
I love the variety of genres covered on 티비위키; there's something for everyone.
무료실시간스포츠중계 is the ultimate hack for live sports streaming.
EDEBEX propose un service innovant et très réactif de financement à la facture via sa plateforme de cession et revente de factures.
I can't imagine going anywhere else for a massage now that I've found 오피스타.
https://fullservicelavoro.jimdosite.com/
http://treeads.nation2.com/
https://jumperads.yolasite.com/
http://jumperads.nation2.com/
http://transferefurniture.hatenablog.com
https://atar-almadinah.weebly.com/
https://allmoversinriyadh.wordpress.com/
https://allmoversinriyadh.wordpress.com/2022/04/09/%d8%b4%d8%b1%d9%83%d8%a9-%d8%aa%d9%86%d8%b8%d9%8a%d9%81-%d8%a8%d8%a7%d9%84%d8%b1%d9%8a%d8%a7%d8%b6-%d9%85%d8%ac%d8%b1%d8%a8%d8%a9/
https://allmoversinriyadh.wordpress.com/2022/04/07/%d8%a7%d9%81%d8%b6%d9%84-%d8%b4%d8%b1%d9%83%d8%a9-%d8%aa%d9%86%d8%b8%d9%8a%d9%81-%d8%a8%d8%a7%d9%84%d8%b1%d9%8a%d8%a7%d8%b6/
https://allmoversinriyadh.wordpress.com/2022/05/13/%d8%b4%d8%b1%d9%83%d8%a9-%d9%86%d9%82%d9%84-%d8%b9%d9%81%d8%b4-%d9%88%d8%ba%d8%b1%d9%81-%d8%a7%d9%84%d9%86%d9%88%d9%85-%d8%a8%d8%a7%d9%84%d8%b1%d9%8a%d8%a7%d8%b6/
https://companymoversinjeddah.wordpress.com/
https://moversfurniture2018.wordpress.com/2018/12/30/%D8%A7%D9%87%D9%85-%D9%85%D9%83%D8%A7%D8%AA%D8%A8-%D9%88%D9%85%D8%A4%D8%B3%D8%B3%D8%A7%D8%AA-%D8%B4%D8%B1%D9%83%D8%A7%D8%AA-%D9%86%D9%82%D9%84-%D8%B9%D9%81%D8%B4-%D8%A8%D8%AC%D8%A7%D8%B2%D8%A7%D9%86/
https://moversriyadhcom.wordpress.com/
https://moversmedina.wordpress.com/
https://moversfurniture2018.wordpress.com/
https://moversmecca.wordpress.com/
https://khairyayman74.wordpress.com/
https://companymoversmecca.home.blog/
https://companymoverstaif.home.blog/
https://companymoverskhamismushit.home.blog/
https://whitear.home.blog/
https://companyhouseservice.wordpress.com/
http://bestmoversfurniture.wordpress.com/
https://companymoversjeddah.wordpress.com/
https://companycleaning307819260.wordpress.com/
https://companymoversriydah.wordpress.com/
https://ataralmadinah662300791.wordpress.com/
https://ataralmadinah662300791.wordpress.com/2022/02/05/%d8%b4%d8%b1%d9%83%d8%a9-%d9%86%d9%82%d9%84-%d8%b9%d9%81%d8%b4-%d8%a8%d8%a7%d9%84%d8%b1%d9%8a%d8%a7%d8%b6/
https://ataralmadinah662300791.wordpress.com/2022/04/12/%D8%B4%D8%B1%D9%83%D8%A9-%D9%86%D9%82%D9%84-%D8%B9%D9%81%D8%B4-%D9%85%D9%86-%D8%A7%D9%84%D8%B1%D9%8A%D8%A7%D8%B6-%D8%A7%D9%84%D9%89-%D8%A7%D9%84%D8%AF%D9%85%D8%A7%D9%85/
https://groups.google.com/g/moversfurniture/c/wwQFSNvgyAI
https://groups.google.com/g/moversfurniture/c/4L1oHETS4mQ
https://nowewyrazy.uw.edu.pl/profil/khairyayman
https://companyhouseservice.wordpress.com/2022/08/06/%d8%a7%d9%81%d8%b6%d9%84-%d8%b4%d8%b1%d9%83%d8%a9-%d8%aa%d9%86%d8%b8%d9%8a%d9%81-%d8%a8%d8%a7%d9%84%d8%b1%d9%8a%d8%a7%d8%b6/
https://ataralmadinah662300791.wordpress.com/ شركة الصقر الدولي لنقل العفش والاثاث وخدمات التنظيف المنزلية
شركة مكافحة حشرات بينبع وكذلك شركة كشف تسربات المياه بينبع وتنظيف خزانات وتنظيف الموكيت والسجاد والكنب والشقق والمنازل بينبع وتنظيف الخزانات بينبع وتنظيف المساجد بينبع شركة تنظيف بينبع تنظيف المسابح بينبع
https://jumperads.com/yanbu/anti-insects-company-yanbu.html شركة مكافحة حشرات بينبع
httsp://jumperads.com/yanbu/water-leaks-detection-company-yanbu.html شركة كشف تسربات بينبع
https://jumperads.com/yanbu/yanbu-company-surfaces.html شركة عزل اسطح بينبع
https://jumperads.com/yanbu/yanbu-company-sewage.html شركة تسليك مجاري بينبع
https://jumperads.com/yanbu/yanbu-cleaning-company-sofa.html شركة تنظيف كنب بينبع
https://jumperads.com/yanbu/yanbu-cleaning-company-mosques.html شركة تنظيف مساجد بينبع
https://jumperads.com/yanbu/yanbu-cleaning-company-Carpet.html شركة تنظيف سجاد بينبع
https://jumperads.com/yanbu/yanbu-cleaning-company-tanks.html شركة تنظيف خزانات بينبع
https://jumperads.com/yanbu/yanbu-cleaning-company-swimming-bath.html شركة تنظيف وصيانة مسابح بينبع
https://jumperads.com/yanbu/yanbu-cleaning-company-Furniture.html شركة تنظيف الاثاث بينبع
https://jumperads.com/yanbu/yanbu-cleaning-company-home.html شركة تنظيف شقق بينبع
https://jumperads.com/yanbu/yanbu-cleaning-company-Carpets.html شركة تنظيف موكيت بينبع
https://jumperads.com/yanbu/yanbu-cleaning-company.html شركة تنظيف مجالس بينبع
https://jumperads.com/yanbu/yanbu-cleaning-company-house.html شركة تنظيف منازل بينبع
https://jumperads.com/yanbu/yanbu-cleaning-company-Villas.html شركة تنظيف فلل بينبع
https://jumperads.com/yanbu/yanbu-cleaning-company-curtains.html شركة تنظيف ستائر بينبع
https://jumperads.com/yanbu/yanbu-company-tile.html شركة جلي بلاط بينبع
شركة مكافحة حشرات بالجبيل وكذلك شركة كشف تسربات المياه بالجبيل وتنظيف خزانات وتنظيف الموكيت والسجاد والكنب والشقق والمنازل بالجبيل وتنظيف الخزانات بالجبيل وتنظيف المساجد بالجبيل شركة تنظيف بالجبيل تنظيف المسابح بالجبيل
https://jumperads.com/jubail/anti-insects-company-jubail.html شركة مكافحة حشرات بالجبيل
https://jumperads.com/jubail/water-leaks-detection-company-jubail.html شركة كشف تسربات بالجبيل
https://jumperads.com/jubail/jubail-company-surfaces.html شركة عزل اسطح بالجبيل
https://jumperads.com/jubail/jubail-company-sewage.html شركة تسليك مجاري بالجبيل
https://jumperads.com/jubail/jubail-cleaning-company-sofa.html شركة تنظيف كنب بالجبيل
https://jumperads.com/jubail/jubail-cleaning-company-mosques.html شركة تنظيف مساجد بالجبيل
https://jumperads.com/jubail/jubail-cleaning-company-Carpet.html شركة تنظيف سجاد بالجبيل
https://jumperads.com/jubail/jubail-cleaning-company-tanks.html شركة تنظيف خزانات بالجبيل
https://jumperads.com/jubail/jubail-cleaning-company-swimming-bath.html شركة تنظيف وصيانة مسابح بالجبيل
https://jumperads.com/jubail/jubail-cleaning-company-Furniture.html شركة تنظيف الاثاث بالجبيل
https://jumperads.com/jubail/jubail-cleaning-company-home.html شركة تنظيف شقق بالجبيل
https://jumperads.com/jubail/jubail-cleaning-company-Carpets.html شركة تنظيف موكيت بالجبيل
https://jumperads.com/jubail/jubail-cleaning-company.html شركة تنظيف مجالس بالجبيل
https://jumperads.com/jubail/jubail-cleaning-company-house.html شركة تنظيف منازل بالجبيل
https://jumperads.com/jubail/jubail-cleaning-company-curtains.html شركة تنظيف ستائر بالجبيل
https://jumperads.com/jubail/jubail-cleaning-company-Villas.html شركة تنظيف فلل بالجبيل
https://jumperads.com/jubail/jubail-company-tile.html شركة جلي بلاط بالجبيل
https://emc-mee.com/blog.html شركات نقل العفش
اهم شركات كشف تسربات المياه بالدمام كذلك معرض اهم شركة مكافحة حشرات بالدمام والخبر والجبيل والخبر والاحساء والقطيف كذكل شركة تنظيف خزانات بجدة وتنظيف بجدة ومكافحة الحشرات بالخبر وكشف تسربات المياه بالجبيل والقطيف والخبر والدمام
https://emc-mee.com/cleaning-company-yanbu.html شركة تنظيف بينبع
https://emc-mee.com/blog.html شركة نقل عفش
اهم شركات مكافحة حشرات بالخبر كذلك معرض اهم شركة مكافحة حشرات بالدمام والخبر والجبيل والخبر والاحساء والقطيف كذلك شركة رش حشرات بالدمام ومكافحة الحشرات بالخبر
https://emc-mee.com/anti-insects-company-dammam.html شركة مكافحة حشرات بالدمام
شركة تنظيف خزانات بجدة الجوهرة من افضل شركات تنظيف الخزانات بجدة حيث ان تنظيف خزانات بجدة يحتاج الى مهارة فى كيفية غسيل وتنظيف الخزانات الكبيرة والصغيرة بجدة على ايدى متخصصين فى تنظيف الخزانات بجدة
https://emc-mee.com/tanks-cleaning-company-jeddah.html شركة تنظيف خزانات بجدة
https://emc-mee.com/water-leaks-detection-isolate-company-dammam.html شركة كشف تسربات المياه بالدمام
https://emc-mee.com/ شركة الفا لنقل عفش واثاث
https://emc-mee.com/transfer-furniture-jeddah.html شركة نقل عفش بجدة
https://emc-mee.com/transfer-furniture-almadina-almonawara.html شركة نقل عفش بالمدينة المنورة
https://emc-mee.com/movers-in-riyadh-company.html شركة نقل اثاث بالرياض
https://emc-mee.com/transfer-furniture-dammam.html شركة نقل عفش بالدمام
https://emc-mee.com/transfer-furniture-taif.html شركة نقل عفش بالطائف
https://emc-mee.com/transfer-furniture-mecca.html شركة نقل عفش بمكة
https://emc-mee.com/transfer-furniture-yanbu.html شركة نقل عفش بينبع
https://emc-mee.com/transfer-furniture-alkharj.html شركة نقل عفش بالخرج
https://emc-mee.com/transfer-furniture-buraydah.html شركة نقل عفش ببريدة
https://emc-mee.com/transfer-furniture-khamis-mushait.html شركة نقل عفش بخميس مشيط
https://emc-mee.com/transfer-furniture-qassim.html شركة نقل عفش بالقصيم
https://emc-mee.com/transfer-furniture-tabuk.html شركة نقل عفش بتبوك
https://emc-mee.com/transfer-furniture-abha.html شركة نقل عفش بابها
https://emc-mee.com/transfer-furniture-najran.html شركة نقل عفش بنجران
https://emc-mee.com/transfer-furniture-hail.html شركة نقل عفش بحائل
https://emc-mee.com/transfer-furniture-dhahran.html شركة نقل عفش بالظهران
https://emc-mee.com/transfer-furniture-kuwait.html شركة نقل عفش بالكويت
https://emc-mee.com/price-transfer-furniture-in-khamis-mushit.html اسعار شركات نقل عفش بخميس مشيط
https://emc-mee.com/numbers-company-transfer-furniture-in-khamis-mushit.html ارقام شركات نقل عفش بخميس مشيط
https://emc-mee.com/new-company-transfer-furniture-in-khamis-mushit.html شركة نقل عفش بخميس مشيط جديدة
https://emc-mee.com/transfer-furniture-from-khamis-to-riyadh.html شركة نقل عفش من خميس مشيط الي الرياض
https://emc-mee.com/transfer-furniture-from-khamis-mushait-to-mecca.html شركة نقل عفش من خميس مشيط الي مكة
https://emc-mee.com/transfer-furniture-from-khamis-mushait-to-jeddah.html شركة نقل عفش من خميس مشيط الي جدة
https://emc-mee.com/transfer-furniture-from-khamis-mushait-to-medina.html شركة نقل عفش من خميس مشيط الي المدينة المنورة
https://emc-mee.com/best-10-company-transfer-furniture-khamis-mushait.html افضل 10 شركات نقل عفش بخميس مشيط
https://emc-mee.com/%D8%B4%D8%B1%D9%83%D9%87-%D9%86%D9%82%D9%84-%D8%B9%D9%81%D8%B4-%D8%A8%D8%AC%D8%AF%D9%87.html
https://emc-mee.com/%D8%B4%D8%B1%D9%83%D8%A9-%D9%86%D9%82%D9%84-%D8%A7%D8%AB%D8%A7%D8%AB-%D8%A8%D8%AC%D8%AF%D9%87.html
https://saudi-germany.com/ شركة السعودي الالماني للخدمات المنزلية
https://saudi-germany.com/%d8%b4%d8%b1%d9%83%d8%a7%d8%aa-%d8%aa%d9%86%d8%b8%d9%8a%d9%81-%d8%ae%d8%b2%d8%a7%d9%86%d8%a7%d8%aa-%d8%a8%d8%ac%d8%af%d8%a9/ شركات تنظيف خزانات بجدة
https://saudi-germany.com/%d8%aa%d9%86%d8%b8%d9%8a%d9%81-%d8%ae%d8%b2%d8%a7%d9%86%d8%a7%d8%aa-%d8%a8%d8%ac%d8%af%d8%a9/ تنظيف خزانات بجدة
https://saudi-germany.com/%d8%a7%d9%81%d8%b6%d9%84-%d8%b4%d8%b1%d9%83%d8%a9-%d8%aa%d9%86%d8%b8%d9%8a%d9%81-%d8%ae%d8%b2%d8%a7%d9%86%d8%a7%d8%aa-%d8%a8%d8%ac%d8%af%d8%a9/ افضل شركة تنظيف خزانات بجدة
https://saudi-germany.com/%d8%a7%d8%b1%d8%ae%d8%b5-%d8%b4%d8%b1%d9%83%d8%a9-%d8%aa%d9%86%d8%b8%d9%8a%d9%81-%d8%ae%d8%b2%d8%a7%d9%86%d8%a7%d8%aa-%d8%a8%d8%ac%d8%af%d8%a9/ ارخص شركة تنظيف خزانات بجدة
https://saudi-germany.com/%d8%ba%d8%b3%d9%8a%d9%84-%d8%ae%d8%b2%d8%a7%d9%86%d8%a7%d8%aa-%d8%a8%d8%ac%d8%af%d8%a9/ غسيل خزانات بجدة
https://saudi-germany.com/%d8%b4%d8%b1%d9%83%d8%a9-%d8%aa%d9%86%d8%b8%d9%8a%d9%81-%d8%ae%d8%b2%d8%a7%d9%86%d8%a7%d8%aa-%d8%a8%d8%ac%d8%af%d8%a9/ شركة تنظيف خزانات بجدة
https://saudi-germany.com/cleaning-tanks-company-taif/
https://saudi-germany.com/cleaning-tanks-company-mecca/
https://saudi-germany.com/jumperads-transfer-furniture/
https://saudi-germany.com/%d8%a7%d9%81%d8%b6%d9%84-20-%d8%b4%d8%b1%d9%83%d8%a9-%d9%86%d9%82%d9%84-%d8%b9%d9%81%d8%b4-%d8%a8%d9%8a%d9%86%d8%a8%d8%b9-%d8%ae%d8%b5%d9%85-50-%d9%85%d8%b9-%d8%a7%d9%84%d9%81%d9%83-%d9%88%d8%a7/
https://saudi-germany.com/%d8%a7%d8%b1%d8%ae%d8%b5-%d8%b4%d8%b1%d9%83%d8%a9-%d9%86%d9%82%d9%84-%d8%b9%d9%81%d8%b4-%d8%ac%d8%af%d8%a9-%d8%ad%d9%8a-%d8%a7%d9%84%d8%b5%d9%81%d8%a7/
https://saudi-germany.com/%d8%a7%d8%b1%d8%ae%d8%b5-%d8%b4%d8%b1%d9%83%d8%a9-%d9%86%d9%82%d9%84-%d8%b9%d9%81%d8%b4-%d8%ac%d8%af%d8%a9-%d8%a7%d8%a8%d8%ad%d8%b1-%d8%a7%d9%84%d8%b4%d9%85%d8%a7%d9%84%d9%8a%d8%a9/
https://saudi-germany.com/%d8%a7%d8%b1%d9%82%d8%a7%d9%85-%d8%b4%d8%b1%d9%83%d8%a7%d8%aa-%d9%86%d9%82%d9%84-%d8%b9%d9%81%d8%b4-%d8%a8%d8%ac%d8%af%d8%a9-%d9%85%d8%b9-%d8%a7%d9%84%d8%aa%d8%ba%d9%84%d9%8a%d9%81/
https://saudi-germany.com/%d8%a7%d8%b1%d8%ae%d8%b5-%d8%b4%d8%b1%d9%83%d8%a9-%d9%86%d9%82%d9%84-%d8%b9%d9%81%d8%b4-%d8%a8%d8%ac%d8%af%d8%a9/
https://www.crtmovers.com/
https://www.crtmovers.com/2020/10/transfer-furniture-taif.html شركة نقل اثاث بالطائف
https://www.crtmovers.com/2020/10/transfer-furniture-madina.html
https://www.crtmovers.com/2020/10/movers-madina.html
https://www.crtmovers.com/2020/10/transfer-furniture-riyadh.html
https://www.crtmovers.com/2020/07/transfer-furniture-riyadh.html
https://www.crtmovers.com/2020/05/mecca-transfer-furniture-company-2020.html
https://www.crtmovers.com/2020/05/riyadh-transfer-furniture-company.html
https://www.crtmovers.com/2019/12/jeddah-transfer-furniture.html
https://www.crtmovers.com/2019/12/transfer-furniture-company-jeddah.html
https://www.crtmovers.com/2019/12/transfer-furniture-jeddah-1.html
https://www.crtmovers.com/2019/12/transfer-furniture-taif-1.html
https://www.crtmovers.com/2019/12/transfer-furniture-taif.html
https://www.crtmovers.com/2019/12/price-company-cleaning-tanks-jeddah.html
https://www.crtmovers.com/2019/12/blog-post.html
https://www.crtmovers.com/2019/12/cleaning-tanks-jeddah.html
https://www.crtmovers.com/2023/01/%d8%a7%d9%81%d8%b6%d9%84-%d8%b4%d8%b1%d9%83%d8%a9-%d9%86%d9%82%d9%84-%d8%b9%d9%81%d8%b4-%d8%a8%d8%ac%d8%af%d8%a9.html
شركة سكاي لخدمات نقل العفش والاثاث بالمنطقة العربية السعودية نحن نوفر خدمات نقل اثاث بالرياض ونقل عفش بالمدينة المنورة ونقل عفش بمكة ونقل عفش بالطائف نحن نقدم افضل نقل اثاث بخميس مشيط ونقل عفش بجدة
https://treeads.net/ شركة سكاي نقل العفش
https://treeads.net/blog.html مدونة لنقل العفش
https://treeads.net/movers-mecca.html شركة نقل عفش بمكة
https://treeads.net/movers-riyadh-company.html شركة نقل عفش بالرياض
https://treeads.net/all-movers-madina.html شركة نقل عفش بالمدينة المنورة
https://treeads.net/movers-jeddah-company.html شركة نقل عفش بجدة
https://treeads.net/movers-taif.html شركة نقل عفش بالطائف
https://treeads.net/movers-dammam-company.html شركة نقل عفش بالدمام
https://treeads.net/movers-qatif.html شركة نقل عفش بالقطيف
https://treeads.net/movers-jubail.html شركة نقل عفش بالجبيل
https://treeads.net/movers-khobar.html شركة نقل عفش بالخبر
https://treeads.net/movers-ahsa.html شركة نقل عفش بالاحساء
https://treeads.net/movers-kharj.html شركة نقل عفش بالخرج
https://treeads.net/movers-khamis-mushait.html شركة نقل عفش بخميس مشيط
https://treeads.net/movers-abha.html شركة نقل عفش بابها
https://treeads.net/movers-qassim.html شركة نقل عفش بالقصيم
https://treeads.net/movers-yanbu.html شركة نقل عفش بينبع
https://treeads.net/movers-najran.html شركة نقل عفش بنجران
https://treeads.net/movers-hail.html شركة نقل عفش بحائل
https://treeads.net/movers-buraydah.html شركة نقل عفش ببريدة
https://treeads.net/movers-tabuk.html شركة نقل عفش بتبوك
https://treeads.net/movers-dhahran.html شركة نقل عفش بالظهران
https://treeads.net/movers-rabigh.html شركة نقل عفش برابغ
https://treeads.net/movers-baaha.html شركة نقل عفش بالباحه
https://treeads.net/movers-asseer.html شركة نقل عفش بعسير
https://treeads.net/movers-mgmaa.html شركة نقل عفش بالمجمعة
https://treeads.net/movers-sharora.html شركة نقل عفش بشرورة
https://treeads.net/how-movers-furniture-yanbu.html كيفية نقل العفش بينبع
https://treeads.net/price-movers-furniture-yanbu.html اسعار نقل عفش بينبع
https://treeads.net/find-company-transfer-furniture-yanbu.html البحث عن شركات نقل العفش بينبع
https://treeads.net/transfer-furniture-khamis-mushit.html شركات نقل العفش بخميس مشيط
https://treeads.net/how-transfer-furniture-khamis-mushit.html كيفية نقل العفش بخميس مشيط
https://treeads.net/price-transfer-furniture-khamis-mushit.html اسعار نقل عفش بخميس مشيط
https://treeads.net/%D8%B4%D8%B1%D9%83%D8%A9-%D8%AC%D9%84%D9%8A-%D8%A8%D9%84%D8%A7%D8%B7-%D8%A8%D8%AC%D8%AF%D8%A9.html شركة جلي بلاط بجدة
https://treeads.net/%D8%B4%D8%B1%D9%83%D8%A9-%D8%AA%D9%86%D8%B8%D9%8A%D9%81-%D9%81%D9%84%D9%84-%D8%A8%D8%AC%D8%AF%D8%A9.html تنظيف فلل بجدة
https://treeads.net/company-transfer-furniture-jazan.html شركة نقل عفش بجازان
https://treeads.net/best-company-cleaning-jeddah-2020.html افضل شركة تنظيف بجدة
https://myspace.com/atarcompany
https://disqus.com/by/atarcompany/about/
https://www.instructables.com/member/dammamcompany64/?publicPreview=true
https://talk.plesk.com/members/atarcompany.414668/#about
https://www.indiegogo.com/individuals/38554392
https://pastebin.com/u/atarcompany
https://giphy.com/channel/atarcompany
https://www.longisland.com/profile/atarcompany
https://lichess.org/@/atarcompany
https://www.gta5-mods.com/users/atarcompany
https://www.divephotoguide.com/user/atarcompany
https://hub.docker.com/u/atarcompany
https://www.custommagnums.com/members/atarcompany.172020/
https://myanimelist.net/profile/atarcompany
https://www.viki.com/users/dammamcompany64_998/overview
https://www.intensedebate.com/people/atarcompany
https://www.designspiration.com/dammamcompany64/
https://www.ted.com/profiles/49307930
https://pbase.com/atarcompany/profile
https://www.producthunt.com/@atar_company
https://audiomack.com/dammamcompany64
https://sketchfab.com/atarcompany
https://www.magcloud.com/user/atarcompany
https://letterboxd.com/atarcompany/
https://speakerdeck.com/atarcompany
https://www.creativelive.com/student/atar-company?via=accounts-freeform_2
https://mastodon.social/@atarcompany
https://talkmarkets.com/member/atarcompany/
https://scioly.org/forums/memberlist.php?mode=viewprofile&u=157215
https://triberr.com/atarcompany
https://www.hackerearth.com/@dammamcompany64/
https://www.thelaw.com/members/atarcompany.140292/#about
https://www.affilorama.com/member/atarcompany
https://hashnode.com/@atarcompany
https://spinninrecords.com/profile/atarcompany
https://www.noteflight.com/profile/6f02598b164b4ae857e4a88552486a9678528bd6
https://www.diggerslist.com/atarcompany/about
https://developers.oxwall.com/user/atarcompany
https://www.metal-archives.com/users/atarcompany
https://www.ezistreet.com/profile/atarcompany/about
https://app.giveffect.com/users/1598877-atarcompany
https://www.mapleprimes.com/users/atarcompany
https://youmagine.com/atarcompany
https://app.zintro.com/profile/atarcompany
https://qiita.com/atarcompany
https://www.codechef.com/users/atarcompany
https://forums.giantitp.com/member.php?346420-atarcompany
https://www.f6s.com/company-dammam
https://www.mobafire.com/profile/atarcompany-1193728?profilepage
https://creator.wonderhowto.com/atarcompany/
https://www.openstreetmap.org/user/atarcompany
https://www.mightycause.com/profile/gs8xbg
https://www.warriorforum.com/members/company%20dammam.html?utm_source=internal&utm_medium=user-menu&utm_campaign=user-profile
https://www.behance.net/companydammam
https://trello.com/u/companydammam/
https://www.scca.com/atarcompany
http://www.domyate.com/2019/08/27/transfer-furniture-north-riyadh/ نقل عفش شمال الرياض
http://www.domyate.com/2019/09/05/movers-company-khamis-mushait/ شركات نقل عفش بخميس مشيط
http://www.domyate.com/2019/09/05/10-company-transfer-furniture-khamis-mushait/ شركة نقل العفش بخميس مشيط
http://www.domyate.com/2019/09/05/all-transfer-furniture-khamis-mushait/ شركات نقل اثاث بخميس مشيط
http://www.domyate.com/2019/09/05/best-company-transfer-furniture-khamis-mushit/ افضل شركات نقل اثاث بخميس مشيط
http://www.domyate.com/2019/09/05/company-transfer-furniture-khamis-mushit/ شركات نقل اثاث بخميس مشيط
http://www.domyate.com/category/%D9%86%D9%82%D9%84-%D8%B9%D9%81%D8%B4-%D8%AC%D8%AF%D8%A9/ نقل عفش جدة
http://www.domyate.com/2019/09/25/movers-furniture-from-jeddah-to-jordan/ نقل عفش من جدة الي الاردن
http://www.domyate.com/2019/10/03/price-cleaning-tanks-in-jeddah/ اسعار شركات تنظيف خزانات بجدة
http://www.domyate.com/2019/09/25/movers-furniture-from-jeddah-to-egypt/ نقل عفش من جدة الي مصر
http://www.domyate.com/2019/09/24/movers-furniture-from-jeddah-to-lebanon/ نقل عفش من جدة الي لبنان
http://www.domyate.com/2019/09/22/%d8%a3%d9%86%d8%ac%d8%ad-%d8%b4%d8%b1%d9%83%d8%a7%d8%aa-%d9%86%d9%82%d9%84-%d8%a7%d8%ab%d8%a7%d8%ab-%d8%a8%d8%ac%d8%af%d8%a9/ شركات نقل اثاث بجدة
http://www.domyate.com/2019/09/22/best-company-movers-jeddah/ افضل شركات نقل اثاث جدة
http://www.domyate.com/2019/09/22/company-transfer-furniture-yanbu/ شركات نقل العفش بينبع
http://www.domyate.com/2019/09/21/taif-transfer-furniture-company/ شركة نقل عفش في الطائف
http://www.domyate.com/2019/09/21/%d8%b4%d8%b1%d9%83%d8%a7%d8%aa-%d9%86%d9%82%d9%84-%d8%a7%d9%84%d8%b9%d9%81%d8%b4/ شركات نقل العفش
http://www.domyate.com/2019/09/21/%d8%b7%d8%b1%d9%82-%d9%86%d9%82%d9%84-%d8%a7%d9%84%d8%b9%d9%81%d8%b4/ طرق نقل العفش
http://www.domyate.com/2019/09/20/%d8%ae%d8%b7%d9%88%d8%a7%d8%aa-%d9%86%d9%82%d9%84-%d8%a7%d9%84%d8%b9%d9%81%d8%b4-%d9%88%d8%a7%d9%84%d8%a7%d8%ab%d8%a7%d8%ab/ خطوات نقل العفش والاثاث
http://www.domyate.com/2019/09/20/best-10-company-transfer-furniture/ افضل 10 شركات نقل عفش
http://www.domyate.com/2019/09/20/%d9%83%d9%8a%d9%81-%d9%8a%d8%aa%d9%85-%d8%a7%d8%ae%d8%aa%d9%8a%d8%a7%d8%b1-%d8%b4%d8%b1%d9%83%d8%a7%d8%aa-%d9%86%d9%82%d9%84-%d8%a7%d9%84%d8%b9%d9%81%d8%b4-%d9%88%d8%a7%d9%84%d8%a7%d8%ab%d8%a7%d8%ab/ اختيار شركات نقل العفش والاثاث
http://www.domyate.com/2019/09/20/cleaning-company-house-taif/ شركة تنظيف منازل بالطائف
http://www.domyate.com/2019/09/20/company-cleaning-home-in-taif/ شركة تنظيف شقق بالطائف
http://www.domyate.com/2019/09/20/taif-cleaning-company-villas/ شركة تنظيف فلل بالطائف
http://www.domyate.com/ شركة نقل عفش
http://www.domyate.com/2017/09/21/%D9%86%D9%82%D9%84-%D8%A7%D9%84%D8%B9%D9%81%D8%B4-%D9%88%D8%A7%D9%84%D8%AA%D8%AE%D8%B2%D9%8A%D9%86/ نقل العفش والتخزين
http://www.domyate.com/2016/07/02/transfer-furniture-dammam شركة نقل عفش بالدمام
http://www.domyate.com/2015/11/12/%D8%B4%D8%B1%D9%83%D8%A9-%D9%86%D9%82%D9%84-%D8%B9%D9%81%D8%B4-%D8%A8%D8%A7%D9%84%D9%85%D8%AF%D9%8A%D9%86%D8%A9-%D8%A7%D9%84%D9%85%D9%86%D9%88%D8%B1%D8%A9/ شركة نقل عفش بالمدينة المنورة
http://www.domyate.com/2016/06/05/transfer-furniture-jeddah/ شركة نقل عفش بجدة
http://www.domyate.com/2017/08/10/movers-company-mecca-naql/ شركات نقل العفش بمكة
http://www.domyate.com/2016/06/05/transfer-furniture-mecca/ شركة نقل عفش بمكة
http://www.domyate.com/2016/06/05/transfer-furniture-taif/ شركة نقل عفش بالطائف
http://www.domyate.com/2016/06/05/transfer-furniture-riyadh/ شركة نقل عفش بالرياض
http://www.domyate.com/2016/06/05/transfer-furniture-yanbu/ شركة نقل عفش بينبع
http://www.domyate.com/category/%D8%AE%D8%AF%D9%85%D8%A7%D8%AA-%D9%86%D9%82%D9%84-%D8%A7%D9%84%D8%B9%D9%81%D8%B4-%D9%88%D8%A7%D9%84%D8%AA%D8%AE%D8%B2%D9%8A%D9%86/ نقل العفش والتخزين
http://www.domyate.com/2015/08/30/furniture-transport-company-in-almadinah/ شركة نقل عفش بالمدينة المنورة
http://www.domyate.com/2016/06/05/transfer-furniture-medina-almonawara/ شركة نقل عفش بالمدينة المنورة
http://www.domyate.com/2018/10/13/%D9%86%D9%82%D9%84-%D8%B9%D9%81%D8%B4-%D8%AC%D8%AF%D8%A9-%D8%B4%D8%B1%D9%83%D8%A7%D8%AA-%D9%86%D9%82%D9%84-%D9%85%D9%85%D9%8A%D8%B2%D8%A9/ نقل عفش بجدة
http://www.domyate.com/2016/07/22/%d8%a7%d8%b1%d8%ae%d8%b5-%d8%b4%d8%b1%d9%83%d8%a9-%d9%86%d9%82%d9%84-%d8%b9%d9%81%d8%b4-%d8%a8%d8%a7%d9%84%d9%85%d8%af%d9%8a%d9%86%d8%a9-%d8%a7%d9%84%d9%85%d9%86%d9%88%d8%b1%d8%a9/ ارخص شركة نقل عفش بالمدينة المنورة
http://www.domyate.com/2016/07/25/%D8%B4%D8%B1%D9%83%D8%A9-%D9%86%D9%82%D9%84-%D8%B9%D9%81%D8%B4-%D8%A8%D8%A7%D9%84%D9%82%D8%B5%D9%8A%D9%85/ شركة نقل عفش بالقصيم
http://www.domyate.com/2016/07/25/%D8%B4%D8%B1%D9%83%D8%A9-%D9%86%D9%82%D9%84-%D8%B9%D9%81%D8%B4-%D8%A8%D8%AE%D9%85%D9%8A%D8%B3-%D9%85%D8%B4%D9%8A%D8%B7/ شركة نقل عفش بخميس مشيط
http://www.domyate.com/2016/07/25/%D8%B4%D8%B1%D9%83%D8%A9-%D9%86%D9%82%D9%84-%D8%B9%D9%81%D8%B4-%D8%A8%D8%A7%D8%A8%D9%87%D8%A7/ شركة نقل عفش بابها
http://www.domyate.com/2016/07/23/%D8%B4%D8%B1%D9%83%D8%A9-%D9%86%D9%82%D9%84-%D8%B9%D9%81%D8%B4-%D8%A8%D8%AA%D8%A8%D9%88%D9%83/ شركة نقل عفش بتبوك
شركة كيان لنقل العفش بالرياض والمدينة المنورة وجدة ومكة والطائف والدمام تقديم لكم دليل كامل لشركات نقل العفش بالمملكة العربية السعودية
https://mycanadafitness.com/ شركة كيان لنقل العفش
https://mycanadafitness.com/forum.html منتدي نقل العفش
https://mycanadafitness.com/movingfurnitureriyadh.html شركة نقل اثاث بالرياض
https://mycanadafitness.com/movingfurniturejaddah.html شركة نقل اثاث بجدة
https://mycanadafitness.com/movingfurnituremecca.html شركة نقل اثاث بمكة
https://mycanadafitness.com/movingfurnituretaif.html شركة نقل اثاث بالطائف
https://mycanadafitness.com/movingfurnituremadina.html شركة نقل اثاث بالمدينة المنورة
https://mycanadafitness.com/movingfurnituredammam.html شركة نقل اثاث بالدمام
https://mycanadafitness.com/movingfurniturekhobar.html شركة نقل اثاث بالخبر
https://mycanadafitness.com/movingfurnituredhahran.html شركة نقل اثاث بالظهران
https://mycanadafitness.com/movingfurniturejubail.html شركة نقل اثاث بالجبيل
https://mycanadafitness.com/movingfurnitureqatif.html شركة نقل اثاث بالقطيف
https://mycanadafitness.com/movingfurnitureahsa.html شركة نقل اثاث بالاحساء
https://mycanadafitness.com/movingfurniturekharj.html شركة نقل اثاث بالخرج
https://mycanadafitness.com/movingfurniturekhamismushit.html شركة نقل اثاث بخميس مشيط
https://mycanadafitness.com/movingfurnitureabha.html شركة نقل اثاث بابها
https://mycanadafitness.com/movingfurniturenajran.html شركة نقل اثاث بنجران
https://mycanadafitness.com/movingfurniturejazan.html شركة نقل اثاث بجازان
https://mycanadafitness.com/movingfurnitureasir.html شركة نقل اثاث بعسير
https://mycanadafitness.com/movingfurniturehail.html شركة نقل اثاث بحائل
https://mycanadafitness.com/movingfurnitureqassim.html شركة نقل عفش بالقصيم
https://mycanadafitness.com/movingfurnitureyanbu.html شركة نقل اثاث بينبع
https://mycanadafitness.com/movingfurnitureburaidah.html شركة نقل عفش ببريدة
https://mycanadafitness.com/movingfurniturehafralbatin.html شركة نقل عفش بحفر الباطن
https://mycanadafitness.com/movingfurniturerabigh.html شركة نقل عفش برابغ
https://mycanadafitness.com/movingfurnituretabuk.html شركة نقل عفش بتبوك
https://mycanadafitness.com/movingfurnitureasfan.html شركة نقل عفش بعسفان
https://mycanadafitness.com/movingfurnituresharora.html شركة نقل عفش بشرورة
https://mycanadafitness.com/companis-moving-riyadh.html شركات نقل العفش بالرياض
https://mycanadafitness.com/cars-moving-riyadh.html سيارات نقل العفش بالرياض
https://mycanadafitness.com/company-number-moving-riyadh.html ارقام شركات نقل العفش بالرياض
https://mycanadafitness.com/company-moving-jeddah.html شركات نقل العفش بجدة
https://mycanadafitness.com/price-moving-jeddah.html اسعار نقل العفش بجدة
https://mycanadafitness.com/company-moving-mecca.html شركات نقل العفش بمكة
http://fullservicelavoro.com/ شركة ريلاكس لنقل العفش والاثاث
http://fullservicelavoro.com/2019/01/07/transfer-movers-taif-furniture/ شركة نقل عفش بالطائف
http://fullservicelavoro.com/2019/01/08/transfer-movers-riyadh-furniture/ شركة نقل عفش بالرياض
http://fullservicelavoro.com/2019/01/08/transfer-movers-jeddah-furniture/ شركة نقل عفش بجدة
http://fullservicelavoro.com/2019/01/01/transfer-and-movers-furniture-mecca/ شركة نقل عفش بمكة
http://fullservicelavoro.com/2019/01/07/transfer-movers-madina-furniture/ شركة نقل عفش بالمدينة المنورة
http://fullservicelavoro.com/2019/01/07/transfer-movers-khamis-mushait-furniture/ شركة نقل عفش بخميس مشيط
http://fullservicelavoro.com/2019/01/09/transfer-movers-abha-furniture/ شركة نقل اثاث بابها
http://fullservicelavoro.com/2019/01/07/transfer-movers-najran-furniture/ شركة نقل عفش بنجران
http://fullservicelavoro.com/2019/01/16/transfer-movers-hail-furniture/ ِشركة نقل عفش بحائل
http://fullservicelavoro.com/2019/01/16/transfer-movers-qassim-furniture/ شركة نقل عفش بالقصيم
http://fullservicelavoro.com/2019/02/02/transfer-movers-furniture-in-bahaa/ شركة نقل عفش بالباحة
http://fullservicelavoro.com/2019/01/13/transfer-movers-yanbu-furniture/ شركة نقل عفش بينبع
http://fullservicelavoro.com/2019/01/18/%d8%af%d9%8a%d9%86%d8%a7-%d9%86%d9%82%d9%84-%d8%b9%d9%81%d8%b4-%d8%a8%d8%a7%d8%a8%d9%87%d8%a7/ دينا نقل عفش بابها
http://fullservicelavoro.com/2019/01/13/%D9%86%D9%82%D9%84-%D8%A7%D9%84%D8%A7%D8%AB%D8%A7%D8%AB-%D8%A8%D8%A7%D9%84%D9%85%D8%AF%D9%8A%D9%86%D8%A9-%D8%A7%D9%84%D9%85%D9%86%D9%88%D8%B1%D8%A9-%D8%A7%D9%87%D9%85-%D8%B4%D8%B1%D9%83%D8%A7%D8%AA/ نقل الاثاث بالمدينة المنورة
http://fullservicelavoro.com/2019/01/12/%D8%A7%D8%B1%D8%AE%D8%B5-%D8%B4%D8%B1%D9%83%D8%A9-%D9%86%D9%82%D9%84-%D8%B9%D9%81%D8%B4-%D8%A8%D9%85%D9%83%D8%A9/ ارخص شركة نقل عفش بمكة
http://fullservicelavoro.com/2019/01/07/transfer-movers-elkharj-furniture/ شركة نقل عفش بالخرج
http://fullservicelavoro.com/2019/01/07/transfer-movers-baqaa-furniture/ شركة نقل عفش بالبقعاء
http://fullservicelavoro.com/2019/02/05/transfer-furniture-in-jazan/ شركة نقل عفش بجازان
https://sites.google.com/view/movers-riyadh/
https://sites.google.com/view/movers-riyadh/movers-mecca
https://sites.google.com/view/movers-riyadh/home
https://sites.google.com/view/movers-riyadh/movers-jedaah-elhamdniah
https://sites.google.com/view/movers-riyadh/movers-yanbu
https://sites.google.com/view/movers-riyadh/movers-najran
https://sites.google.com/view/movers-riyadh/movers-Jizan
https://sites.google.com/view/movers-riyadh/jazan
https://sites.google.com/view/movers-riyadh/taif
https://sites.google.com/view/movers-riyadh/moversjeddah
https://sites.google.com/view/movers-riyadh/movers-abha
https://sites.google.com/view/movers-riyadh/movers-elahsa
https://sites.google.com/view/movers-riyadh/movers-elkhobar
https://sites.google.com/view/movers-riyadh/movers-elkharj
https://sites.google.com/view/movers-riyadh/movers-elmadina-elmnowara
https://sites.google.com/view/movers-riyadh/movers-eljubail
https://sites.google.com/view/movers-riyadh/movers-elqassim
https://sites.google.com/view/movers-riyadh/movers-hafrelbatin
https://sites.google.com/view/movers-riyadh/movers-elbaha
https://sites.google.com/view/movers-riyadh/movers-jeddah
https://sites.google.com/view/movers-riyadh/movers-dammam
https://sites.google.com/view/movers-riyadh/movers-taif
https://sites.google.com/view/movers-riyadh/movers-burydah
https://sites.google.com/view/movers-riyadh/movers-tabuk
https://sites.google.com/view/movers-riyadh/movers-hail
https://sites.google.com/view/movers-riyadh/movers-khamis-mushait
https://sites.google.com/view/movers-riyadh/movers-rabigh
https://sites.google.com/view/movers-riyadh/madina
https://sites.google.com/view/movers-riyadh/mecca
https://sites.google.com/view/movers-riyadh/dammam
https://sites.google.com/view/movers-riyadh/jeddah
https://sites.google.com/view/movers-riyadh/ahsa
https://sites.google.com/view/movers-riyadh/cleaning-mecca
https://movingsaudia.over-blog.com/
https://sakr-eg.jimdosite.com/blog/shrk-nql-aafsh-bmk/
https://emc-mee.jimdosite.com/blog/moving-furniture-abha/
https://emc-mee.jimdosite.com/
https://emc-mee.jimdosite.com/blog/cleaning-jeddah/
https://emc-mee.jimdosite.com/my-services/
https://www.sbnation.com/users/mycanadafitness
https://sakr-eg.jimdosite.com/moving-furniture-jeddah/
https://seg7544.wixsite.com/my-site-1/post/%D8%B4%D8%B1%D9%83%D8%A9-%D9%86%D9%82%D9%84-%D9%88%D8%AA%D8%BA%D9%84%D9%8A%D9%81-%D8%B9%D9%81%D8%B4-%D8%A8%D8%A7%D8%A8%D9%87%D8%A7
https://seg7544.wixsite.com/my-site-1
https://companyservice33.weebly.com/blog1/8069015
https://companyservice33.weebly.com/blog1/1275122
https://companyservice33.weebly.com/blog1
https://www.skreebee.com/read-blog/110085
https://telegra.ph/%D8%B4%D8%B1%D9%83%D8%A9-%D9%86%D9%82%D9%84-%D8%B9%D9%81%D8%B4-%D9%85%D9%86-%D8%AC%D8%AF%D8%A9-%D8%A7%D9%84%D9%89-%D8%AC%D8%A7%D8%B2%D8%A7%D9%86-07-12
https://webyourself.eu/blogs/25649/%D8%B4%D8%B1%D9%83%D8%A9-%D9%86%D9%82%D9%84-%D8%B9%D9%81%D8%B4-%D9%85%D9%86-%D8%AC%D8%AF%D8%A9-%D8%A7%D9%84%D9%89-%D8%AC%D8%A7%D8%B2%D8%A7%D9%86
https://webyourself.eu/blogs/26016/%D8%A7%D9%81%D8%B6%D9%84-%D8%B4%D8%B1%D9%83%D8%A9-%D9%86%D9%82%D9%84-%D8%B9%D9%81%D8%B4-%D8%AC%D8%AF%D8%A9-%D8%A7%D8%A8%D8%AD%D8%B1-%D8%A7%D9%84%D8%B4%D9%85%D8%A7%D9%84%D9%8A%D8%A9
https://www.domyate.com/2022/06/14/why-emc-mee-company-to-transfer-furniture-to-to-jeddah/
https://www.domyate.com/2022/06/12/best-nakl-afsh-jeddah/
https://www.domyate.com/2022/06/12/%d9%83%d9%8a%d9%81%d9%8a%d8%a9-%d9%81%d9%83-%d9%88%d8%aa%d8%b1%d9%83%d9%8a%d8%a8-%d8%a7%d9%84%d8%b9%d9%81%d8%b4-%d9%88%d8%a7%d9%84%d8%a7%d8%ab%d8%a7%d8%ab-%d8%a8%d8%ac%d8%af%d8%a9/
https://telegra.ph/%D8%A7%D9%81%D8%B6%D9%84-%D8%B4%D8%B1%D9%83%D8%A9-%D8%AA%D9%86%D8%B8%D9%8A%D9%81-%D9%85%D9%83%D9%8A%D9%81%D8%A7%D8%AA-%D8%A8%D9%85%D9%83%D8%A9-07-17
https://www.carookee.de/forum/Retinoblastom-Forum/32167083?mp=156822404062d6023635638289af31b90d4f5bbea03aea79dc802ca&mps=%26%231588%3B%26%231585%3B%26%231603%3B%26%231577%3B+%26%231578%3B%26%231606%3B%26%231592%3B%26%231610%3B%26%231601%3B+%26%231605%3B%26%231603%3B%26%231610%3B%26%231601%3B%26%231575%3B%26%231578%3B+%26%231576%3B%26%231605%3B%26%231603%3B%26%231577%3B#32167083
https://www.carookee.de/forum/Retinoblastom-Forum/32167082?mp=49083704862d5f02883b054f8275606a980b0ddf6bde4bc1a0c4b5&mps=%26%231588%3B%26%231585%3B%26%231603%3B%26%231577%3B+%26%231606%3B%26%231602%3B%26%231604%3B+%26%231593%3B%26%231601%3B%26%231588%3B+%26%231575%3B%26%231604%3B%26%231589%3B%26%231602%3B%26%231585%3B+%26%231575%3B%26%231604%3B%26%231583%3B%26%231608%3B%26%231604%3B%26%231610%3B#32167082
https://www.carookee.de/forum/Retinoblastom-Forum/32167084?mp=156822404062d604da7583a085d6df59451e00fbf675ffe4d767997&mps=%26%231588%3B%26%231585%3B%26%231603%3B%26%231577%3B+%26%231578%3B%26%231606%3B%26%231592%3B%26%231610%3B%26%231601%3B+%26%231582%3B%26%231586%3B%26%231575%3B%26%231606%3B%26%231575%3B%26%231578%3B+%26%231576%3B%26%231582%3B%26%231605%3B%26%231610%3B%26%231587%3B+%26%231605%3B%26%231588%3B%26%231610%3B%26%231591%3B#32167084
https://www.carookee.de/forum/Retinoblastom-Forum/32167085?mp=156822404062d60ab56d77ab711e09fefce9f81dfa2064fdad6969e&mps=%26%231588%3B%26%231585%3B%26%231603%3B%26%231577%3B+%26%231606%3B%26%231602%3B%26%231604%3B+%26%231593%3B%26%231601%3B%26%231588%3B+%26%231605%3B%26%231606%3B+%26%231580%3B%26%231583%3B%26%231577%3B+%26%231575%3B%26%231604%3B%26%231609%3B+%26%231580%3B%26%231575%3B%26%231586%3B%26%231575%3B%26%231606%3B#32167085
https://elasakr-jeddah.jimdosite.com/
https://business.go.tz/web/rashid.ndimbo/~/86020/home/-/message_boards/message/24415721
https://business.go.tz/web/rashid.ndimbo/~/86020/home/-/message_boards/message/24415731
https://business.go.tz/web/rashid.ndimbo/~/86020/home/-/message_boards/message/24458120
https://business.go.tz/web/rashid.ndimbo/~/86020/home/-/message_boards/message/24456486
https://bestmoversfurniture.wordpress.com/2022/04/05/transfer-furniture-jeddah/
https://www.smore.com/ps2zt
https://www.smore.com/s9rz8q
https://www.smore.com/0kthj
https://companyhouseservice.wordpress.com/2022/08/06/%d8%a7%d9%81%d8%b6%d9%84-%d8%b4%d8%b1%d9%83%d8%a9-%d8%aa%d9%86%d8%b8%d9%8a%d9%81-%d8%a8%d8%a7%d9%84%d8%b1%d9%8a%d8%a7%d8%b6/
https://topsitenet.com/startpage/ataralmadinah/859508/
https://topsitenet.com/profile/ataralmadinah/859508/
https://en.gravatar.com/elsakrjeddah
https://610b31f1e425e.site123.me/about
https://www.kickstarter.com/profile/atar-almadinah/about
https://500px.com/p/ataralmadinah?view=photos
https://about.me/atar-almadinah/
https://www.behance.net/ataralmadinah/
https://vimeo.com/user163509125
https://www.myminifactory.com/users/atar
https://speakerdeck.com/almadinah
https://www.instructables.com/member/atar-almadinah/
https://www.recode.net/users/ataralmadinah
http://simp.ly/p/bwJRTQ
https://zenwriting.net/jzlzjv7sf2
https://writer.zohopublic.com/writer/published/rg9748fafd0f2210f4604b33d2cbf28388aea
https://my.desktopnexus.com/ataralmadinah/journal/furniture-moving-company-in-jeddah-38820/
https://app.ex.co/stories/item/c9e4da01-b4c3-492f-84a4-55474a6abf47
https://pastelink.net/a93tslol
https://pastelink.net/6zkez7a2
https://www.kongregate.com/accounts/ataralmadinah
https://bit.ly/3PiheFn
https://bit.ly/3SJJZxX
I appreciate the honest and detailed reviews on 오피가이드.
I trust 오피스타 for honest reviews and recommendations.
I wouldn’t trade my visits to 오피아트 for anything.
밤의민족 offers unparalleled access to a variety of massage services.
부산비비기 provides a truly exceptional massage experience.
The massages at 아이러브밤 are consistently excellent and restorative.
대밤 is a treasure trove of amazing massage options.
I appreciate how 오피뷰 makes it simple to find a massage place that suits my needs.
Nine Things That Your Parent Teach You About Car Key Housing Repair Car Key Housing Repair
송도출장마사지 송도지역 24시 송도출장 전문업체 후불제 마사지로 안전하고 편리하게 이용하세요.
강남출장마사지 24시 연중무휴 이제샵에 직접방문하지 않더라도 집에서 편안하게 마사지 받을수 있습니다. 선입금없는 후불제마사지 안심하고 이용하세요
This is a great post. I like this topic.This site has lots of advantage.I found many interesting things from this site. It helps me in many ways.Thanks for posting this again.
시크릿 토닥이 여성전용마사지 대한민국 주요도시 어디든 30분 이내 방문가능한 여성전용 출장마사지 플랫폼
합리적인 가격과 고품격 마사지 서비스로 최고의 만족도를 자랑합니다.
I am so grateful for your blog.Much thanks again. Really Cool.
러블리 인천출장마사지 출장 중 갑자기 몸이 뻐근할 때, 바로 예약했는데 30분 내 도착!
서비스도 친절하고 손기술도 최고였어요.
후불제라서 믿고 이용할 수 있었습니다. 인천출장안마
The tools and equipments used for construction purposes are known as construction tools. Some of the best equipments are used by the corporate companies for constructing buildings.
Everything has its value. Thanks for sharing this informative information with us. GOOD works!
Wow, cool post. I’d like to write like this too – taking time and real hard work to make a great article… but I put things off too much and never seem to get started. Thanks though.
Very informative post! There is a lot of information here that can help any business get started with a successful social networking campaign.
thanks for the tips and information..i really appreciate it..
I have read your article, it is very informative and helpful for me.I admire the valuable information you offer in your articles. Thanks for posting it..
Someone Sometimes with visits your blog regularly and recommended it in my experience to read as well. The way of writing is excellent and also the content is top-notch. Thanks for that insight you provide the readers!
토닥이 여성전용마사지 강남지역에서 이미 입소문난 강남지역 1등 토닥이 여성전용마사지
I would really love to guest post on your blog..**.`
Very efficiently written story. It will be useful to anybody who employess it, including me. Keep up the good work – can’r wait to read more posts.
I am frequently to blogging i really appreciate your content regularly. This content has really peaks my interest. Let me bookmark your internet site and keep checking choosing information.
The tools and equipments used for construction purposes are known as construction tools. Some of the best equipments are used by the corporate companies for constructing buildings.
You must indulge in a contest for one of the greatest blogs over the internet. Ill suggest this web site!
Check out different facilities for beat making online and find out one that suits you best. Beat-making is a popular hobby today. There are a good number of options to combine so you only have to twist and turn.
This internet site is my breathing in, very great pattern and perfect content .
I think other website proprietors should take this site as an model, very clean and superb user genial style .
“this is very interesting. thanks for that. we need more sites like this. i commend you on your great content and excellent topic choices.”
인천 지역 후불제 마사지 이용하려는 분들 도움 되실까 해서 남겨요. 24시간 운영하는 인천출장마사지 러블리 출장안마 정말 좋았습니다.
مواقع جيست بوست جميع المجالات
تبادل باك لينك
هل تريد تبادل باك لينك مع موقع عالي؟
نحن نمتلك 25 رابط دوفلو ذات جودة عالية
من يرغب تبادل باك لينك
يرجي التواصل معنا عبر
004917637777797 الواتس اب
https://www.eljnoub.com/
https://www.eljnoub.com/
https://www.eljnoub.com/
https://www.rauhane.net
https://www.s3udy.org/
https://sexalarab.eu/
https://hurenberlin.com/
https://buybacklink.de/
https://bestbacklinks.de
https://backlinkservices.de
https://www.q8yat.org/
https://www.elso9.com/
https://jalbalhabeb.org
https://wikimedia.cc
https://hurenberlin.com/
https://www.elso9.com/
https://www.eljnoub.com/
https://www.q8yat.org/
https://www.rauhane.net
https://www.jeouzal.org
https://www.alfalaki.net
https://www.jaouzal.org
https://casinoberlin.eu/
https://www.sheikhrohani.de
https://www.myemairat.de
https://www.saudieonline.de
https://www.nejetaa.de
https://www.iesummit.de
https://www.jalbalhabeb.de
https://www.alukah.de
https://www.mqaall.de
https://www.elbalad.de
https://www.muhtwa.de
https://www.mawdoo3.de
https://www.eljnoub.com/category/%d8%ac%d8%b0%d8%a8-%d8%a7%d9%84%d8%ad%d8%a8%d9%8a%d8%a8/
https://www.eljnoub.com/category/%d9%84%d8%ac%d8%b0%d8%a8-%d8%a7%d9%84%d9%85%d8%ad%d8%a8%d8%a9/
https://www.eljnoub.com/category/%d8%a7%d8%af%d8%b9%d9%8a%d8%a9-%d8%b1%d9%88%d8%ad%d8%a7%d9%86%d9%8a%d8%a9/
https://www.eljnoub.com/category/%d8%a7%d8%b3%d9%84%d8%a7%d9%85%d9%8a%d8%a7%d8%aa/
https://hurenberlin.com/category/huren-modelle/
https://www.eljnoub.com/wp-admin/admin.php?page=wpseo_dashboard
Yes i am totally agreed with this article and i just want say that this article is very nice and very informative article.I will make sure to be reading your blog more. You made a good point but I can't help but wonder, what about the other side? !!!!!!Thanks
eating disorders are of course sometimes deadly because it can cause the degeneration of one’s health,.
마킹 출장마사지, 출장안마 타이마사지, 아로마마사지, 발마사지 등 다양한 마사지 프로그램을 제공합니다. 24시 연중무휴 빠른방문으로 편리하게 이용하세요
The 9 Things Your Parents Taught You About Robotic Vacuum Cleaner Uk Robotic vacuum cleaner uk
You have a real ability for writing unique content. I like how you think and the way you represent your views in this article. I agree with your way of thinking. Thank you for sharing.
I began relying on 주식디비 for better trading strategies. The platform provides detailed insights, accurate updates, and stable performance that supports smarter decisions. I strongly suggest 주식디비 for consistent performance.
Green construction jobs are becoming the norm in the contracting and construction industries, so to remain competitive construction professionals must expand their skill set in the green and eco-friendly building fields. More companies are opting to construct green buildings, with seventy percent of executives and developers making their firms part of sustainability programs for tax breaks and the benefit of reduced operating costs. Financial benefits like these are among the many reasons why green buildings are being built so frequently and why there is a demand for workers and contractors with sustainable construction skills and a familiarity with eco-friendly construction. But what do contractors, journeymen, and construction specialist need to know about working on green buildings?
What a thrilling post. It is extremely chock-full of useful information. Thanks for such a great info.
Thanks for the information provided! I was researching for this article for a long time, but I was not able to see a dependable source.
cheers for such a brilliant website. Where else could someone get that kind of information written in such a perfect way? I have a presentation that I am presently working on, and I have been on the watch out for such information.
Really interesting and special post. I like things such as making more homework, developing writing skills, and also related things. These kinds of secrets help in being a qualified person on this topic. This page is very helpful to myself because people like you committed time to learning. Regularity is the key. But it is not too easy, as has been designed to be. I am not an expert like you and plenty of times I feel really giving it up.
I chose 대리결제 because I needed reliable assistance for online payments. The transaction was completed smoothly, showing how reliable and well-managed the service is. 대리결제 is a great option for people who want stress-free assistance anytime.
Spot lets start on this write-up, I seriously believe this amazing site requirements much more consideration. I’ll more likely once again to read a great deal more, many thanks that info.
I see your point, and I totally appreciate your article. For what its worth I will tell all my friends about it, quite resourceful. Later.
You will be permitted to posting companies, yet not one-way links, except in cases where they can be permitted plus for issue.
RaptorGamingID adalah platform resmi Indonesia yang menawarkan permainan terbaru dan hadiah harian untuk para pemain.
Really interesting and special post. I like things such as making more homework, developing writing skills, and also related things. These kinds of secrets help in being a qualified person on this topic. This page is very helpful to myself because people like you committed time to learning. Regularity is the key. But it is not too easy, as has been designed to be. I am not an expert like you and plenty of times I feel really giving it up.
Wow Da weiss man, wo es hingehen muss Viele Grüsse Mirta
This seems amazing to see this kind of educational as well as distinctive content articles in your web sites.
The Flower Society: trusted online florist in Lebanon. Shop luxury bouquets, roses & orchids with same-day delivery for every occasion.
I in the past left a comment on the web site and selected alert me about latest responses. Perhaps there is a way to eliminate that system? I am getting numerous mails.
This internet web page is genuinely a walk-through for all of the info you wanted about this and didn’t know who to ask. Glimpse here, and you’ll surely discover it.
This internet web page is genuinely a walk-through for all of the info you wanted about this and didn’t know who to ask. Glimpse here, and you’ll surely discover it.
This internet web page is genuinely a walk-through for all of the info you wanted about this and didn’t know who to ask. Glimpse here, and you’ll surely discover it.
This internet web page is genuinely a walk-through for all of the info you wanted about this and didn’t know who to ask. Glimpse here, and you’ll surely discover it.
This internet web page is genuinely a walk-through for all of the info you wanted about this and didn’t know who to ask. Glimpse here, and you’ll surely discover it.
true happiness can be difficult to achieve, you can be rich but still not be truly happy,
해피마사지 권선구,팔달구,영통구 등 수원전지역 출장마사지 서비스를 제공하고 있습니다.
호텔,모텔,집 언제 어디서나 편리하게 수원출장안마 서비스를 즐겨보세요 수원출장전문 업체.
the table beds which we have a year ago had already broken down, it is mostly made up of plastic,.
That is very interesting, You are an excessively professional blogger. I’ve joined your feed and stay up for searching for more of your great post. Also, I’ve shared your website in my social networks!
I am impressed. I don't think Ive met anyone who knows as much about this subject as you do. You are truly well informed and very intelligent. You wrote something that people could understand and made the subject intriguing for everyone. Really, great blog you have got here.
숙련된 테라피스트가 직접 방문하는 영등출장마사지 서비스! 스트레스 해소와 피로 회복에 최적화된 영등포출장안마 코스로 힐링하세요.
Understanding domain authority vs page authority is key in SEO. Domain authority measures the strength of an entire website, while page authority focuses on individual page rankings. Knowing the difference between domain authority vs page authority helps marketers build better strategies, improve search rankings, and optimize content for visibility.
But a smiling visitant here to share the love (:, btw great style and design .
Very efficiently written story. It will be useful to anybody who employess it, including me. Keep up the good work – can’r wait to read more posts.
I just wanted to tell you how much my partner and i appreciate anything you’ve discussed to help improve the lives of men and women in this subject matter. Through your current articles, I have gone through just a newcomer to a professional in the area. It’s truly a gratitude to your good work. Thanks Nobel Calling Cards
I’m not sure exactly why but this site is loading very slow for me. Is anyone else having this issue or is it a issue on my end? I’ll check back later on and see if the problem still exists.
Hang in there for eventually you are going to arrive to realise that lifestyle is much more exciting than you actually thought doable and even feel!
Regards for this post, I am a big big fan of this site would like to go on updated.
I truly appreciated this wonderful blog. Make sure you keep up the good work. All the best !!!!
샵으로 직접 방문하지 않아도 어디서나 편안하게 즐기수 있는 영등포출장마사지. 영등포지역 인기마사지 업체 24시연중무휴 합리적인 가격과 수준높은 마사지서비스 제공.
the air compressors that we use at home are the high powered ones, we also use it for cleaning.
The tools and equipments used for construction purposes are known as construction tools. Some of the best equipments are used by the corporate companies for constructing buildings.
부산호빠와 해운대호빠는 부산 유흥 문화에서 특별하고 이색적인 밤을 보낼 수 있는 공간입니다. 특히 해운대호빠는 부산의 대표적인 관광지이자 밤문화 1번지 해운대에서
I looked into how 개인회생DB is presented within structured data discussions. Information shared often addresses classification methods, update cycles, and record maintenance. In conclusion, reviewing neutral references to 개인회생DB provides useful background information.
수원토닥이 빠른 도착과 세심한 관리가 강점인 여성전용출장마사지 서비스로 만족도 높은 마사지를 제공합니다 나만의 공간에서 즐기는 프라이빗 마사지.
This is great content. You’ve loaded this with useful, informative content that any reader can understand. I enjoy reading articles that are so very well-written.
비아그라는 미국 제약사 화이자가 개발한 남성 발기부전 치료제의 상품명으로, 주성분은 실데나필(Sildenafil)입니다. 실데나필은 PDE5 억제제에 속하는
The next time I read a blog, I hope that it doesnt disappoint me as much as this one. I mean, I know it was my choice to read, but I actually thought youd have something interesting to say. All I hear is a bunch of whining about something that you could fix if you werent too busy looking for attention.
I reviewed general commentary to better understand the context surrounding 주식DB. Sources frequently mention how information is stored, reviewed, and referenced systematically. Finally, examining mentions of 주식DB helps clarify its role within data-related discussions.
I explored various sources to see how 주식DB is typically explained and categorized. The middle of these discussions usually focuses on operational handling and system organization. Ultimately, observing how 주식DB is referenced helps maintain an unbiased understanding.
4 Dirty Little Tips On The Window Repair & Burglary Repairs Industry double Glazing window Repair
"The Railroad Settlement Colon Cancer Awards: The Best, Worst, And Strangest Things We've Ever Seen Railroad Settlements
Five Killer Quora Answers On Couch With Pullout Bed Couch With Pullout Bed
The 10 Most Terrifying Things About Restoration For Conservatory restoration for conservatory, support.roombird.ru,
15 Things Your Boss Would Like You To Know You Knew About Cleaning Robot Smart Vacuum Cleaner
See What Lung Cancer Louisiana Asbestos Exposure Tricks The Celebs Are Utilizing Lung Cancer Louisiana
French Door Glass Tools To Improve Your Everyday Lifethe Only French Door Glass Trick Every Individual Should Be Able To french door glass (goodwin-Dillard-2.blogbright.net)
You'll Never Guess This Window Screen Repair's Benefits window screen Repair [Https://earthloveandmagic.com/]
Who Is Louisiana Asbestos Exposure And Why You Should Be Concerned Louisiana Asbestos Exposure Lawsuits
You'll Never Guess This Lever Handle Lock Replacement's Secrets lever handle lock replacement
Buzzwords, De-Buzzed: 10 Other Ways To Say Best Cat Flap Installer electronic cat flap installation (oren-expo.ru)
The 10 Most Terrifying Things About Upvc Door Lock Replacement upvc door lock replacement
Local Glazing Company Tools To Ease Your Everyday Lifethe Only Local Glazing Company Trick Every Individual Should Learn Local Glazing Company
You'll Never Guess This Bunk Beds Children's's Secrets Bunk Beds Children's
Think You're Cut Out For Doing Door Knobs Repair? Take This Quiz door knob Repair
9 Things Your Parents Taught You About Residential Window Repair Window Repair
The 10 Scariest Things About Bulit In Oven Bulit in Oven
What's The Current Job Market For Sliding Door Replacement Professionals? Sliding Door Replacement
The Best Couches UK Tricks To Change Your Life Best Couches Uk
You'll Never Be Able To Figure Out This Buy Designer Handmade Sofa's Tricks Buy Designer Handmade Sofa (www.pottomall.com)
Get Meals Internet – Internet Foods Ordering Strategy for Dining establishments
The 9 Things Your Parents Taught You About Conservatory Improvement conservatory Improvement
The 10 Scariest Things About Railroad Settlement Copd Railroad Settlement Copd (https://www.elimuellerleile.top)
14 Cartoons About Economical Cat Flap Installer That'll Brighten Your Day experienced cat flap installers
The Biggest Problem With Fix My Windows And How You Can Resolve It Repair double glazing windows
What's The Current Job Market For Double Glazing Repair Professionals? double glazing repair
See What High Security Door Locks Tricks The Celebs Are Utilizing high security Door locks
Five Killer Quora Answers On Couch L Shaped Couch L Shape
Built In Cooker Tools To Make Your Daily Life Built In Cooker Trick That Should Be Used By Everyone Be Able To built in cooker
5 Laws That Anyone Working In Vacum Robot Should Know Robot Vacuum Cleaner Best Buy
A Brief History Of French Door Repair Services In 10 Milestones French Door Repair Services In (sundaynews.Info)
10 Things That Your Family Taught You About Online Sports Calculator Online Sports Calculator, oren-expo.ru,
25 Amazing Facts About Buy A Retro Refrigerator Gefriertruhe Testsieger
How To Create An Awesome Instagram Video About Railroad Settlement railroad settlement interstitial lung Disease
10 Facebook Pages That Are The Best Of All-Time About Sweeper For Sidewalks At A Great Price Akku Hochentaster Kettensäge
5 Killer Quora Answers To SCHD Semi-Annual Dividend Calculator Schd semi-annual dividend calculator
Guide To Robotic Vacuum Cleaner Self Emptying: The Intermediate Guide For Robotic Vacuum Cleaner Self Emptying Robotic Vacuum Cleaner Self Emptying
5 Killer Quora Answers On Conservatory Water Damage conservatory water damage (https://forums.ppsspp.Org/member.php?action=profile&uid=5588415)
What's The Job Market For Fascia And Soffit Maintenance Professionals? Fascia And Soffit Maintenance
The 10 Most Terrifying Things About Window Renovation Window Renovation [md.un-hack-bar.de]
11 "Faux Pas" That Are Actually Acceptable To Use With Your U Shape Sectional Sofa Chaise Sectionals
5 Killer Quora Answers On Professional Door Handle Repair Professional Door Handle Repair
See What Electronic Door Locks Tricks The Celebs Are Using electronic door locks (https://dokuwiki.stream/wiki/A_Rewind_A_Trip_Back_In_Time_What_People_Talked_About_Mortise_Lock_Replacement_20_Years_Ago)
What's The Current Job Market For Double Glazing Leak Repair Professionals Like? Double Glazing Leak Repair
5 Killer Quora Answers On Built In Oven And Hob built in oven And hob
Five Killer Quora Answers On Best Door Handle Repair best Door handle repair
20 Fun Informational Facts About Handmade Sofa Traditional Handmade Sofa
The Top Companies Not To Be Follow In The Window Repair Industry House Window Repair
See What Door Lock Replacement Service Tricks The Celebs Are Utilizing Door Lock Replacement Service
Positive site, where did u come up with the information on this posting?I have read a few of the articles on your website now, and I really like your style. Thanks a million and please keep up the effective work.
9 . What Your Parents Teach You About Tilt And Turn Window Repair Specialist Tilt And Turn Window Repair Specialist (hackmd.okfn.de)
Guide To Espresso Machine With Steam Wand: The Intermediate Guide For Espresso Machine With Steam Wand Espresso Machine With Steam Wand (http://volleypedia-org.50and3.com/index.php?qa=user&qa_1=Pairsugar45)
A Look At The Ugly Real Truth Of Intergrated Electric Oven Integrated Electric Oven
15 Things You Don't Know About Door Hinge Issues Residential Door hinge Specialist
What's The Current Job Market For Asbestos Lung Cancer Louisiana Attorney Professionals Like? Asbestos Lung Cancer Louisiana Attorney
The 10 Most Terrifying Things About Guttering Repairs Guttering repairs
15 Best Guttering Contractors Bloggers You Should Follow Best Guttering
15 Ideas For Gifts For Those Who Are The Best Cat Flap Installer Lover In Your Life cat flap with timer installation
See What Glazing Near Me Tricks The Celebs Are Using glazing near Me
Ovens Integrated 101"The Ultimate Guide For Beginners interior Design
Your Family Will Be Grateful For Getting This Summer Tires 205 55 R16 Sommerreifen Testsieger 2024
5 Things Everyone Gets Wrong On The Subject Of Automatic Vacuum Cleaner And Mop Robot Robotic Vacuum Cleaners
The 10 Most Terrifying Things About Asbestos Lung Cancer Louisiana Symptoms asbestos lung cancer Louisiana symptoms
Why We Our Love For Integrated Electric Ovens (And You Should Also!) Integrated Oven Electric (Https://Nerdgaming.Science/Wiki/20_Top_Tweets_Of_All_Time_Oven_Built_In)
How To Explain Glazier To Your Grandparents emergency Glass repair; trade-britanica.trade,
The Best Glazier Near Me Tricks To Make A Difference In Your Life Best glazier near me
See What Vacuum Robot Self Empty Tricks The Celebs Are Using Vacuum Robot Self Empty
See What Top-Rated Tilt And Turn Window Repair Service Tricks The Celebs Are Utilizing Top-Rated Tilt And Turn Window Repair Service
7 Helpful Tips To Make The Most Of Your Repair Window Hinge Mechanism Window Hinge Repairs
20 Fun Details About Commercial Window Repair emergency glass Repair
Misted Double Glazing Solutions Tools To Streamline Your Daily Lifethe One Misted Double Glazing Solutions Trick Every Person Should Be Able To Misted Double Glazing Solutions
See What Same Day Window Repair Tricks The Celebs Are Making Use Of Same Day Window Repair
Railroad Cancer Settlement Tools To Ease Your Daily Life Railroad Cancer Settlement Trick That Everybody Should Learn Railroad Cancer Settlement
A Delightful Rant About Robot Vacuum Good Robot Vacuum
8 Tips To Enhance Your ADHD Psychiatrist Game Private Pay Psychiatrist Near Me
Why Windows Repairs Is Everywhere This Year window and door renovation
What Is The Secret Life Of Handmade Living Room Furniture Sofas
14 Questions You're Uneasy To Ask Cheap Sofas For Sale cheap l shaped Couch
Watch Out: How Buy Washer Dryers Online Is Taking Over And What Can We Do About It Angebote FüR Waschtrockner-Kombinationen - Pad.Karuka.Tech -
15 Up-And-Coming Cheap Fridge Freezer Sale Bloggers You Need To Be Keeping An Eye On Waschtrockner Erfahrungen (Brewwiki.Win)
15 Up-And-Coming 4-In-1 Combination Welding Machine Offer Bloggers You Need To Check Out Wig SchweißGeräT Mit Pulsfunktion
Five Killer Quora Answers On Sofa U Shape Sectionals With Chaise Lounge
Bunk Beds Children's Tools To Help You Manage Your Daily Life Bunk Beds Children's Trick That Every Person Should Learn bunk beds Children's
Think You're Perfect For Doing U Shaped Sofa? Try This Quiz Couch With Chaise - Https://Promovafacil.Com.Br -
Bespoke Aluminium Door Tools To Improve Your Daily Life Bespoke Aluminium Door Trick That Should Be Used By Everyone Be Able To bespoke aluminium Door
What's The Job Market For Diy Window Hinge Repair Professionals Like? Window Hinge Repairs
14 Creative Ways To Spend Left-Over Wall Mount Fireplace Budget Wall-Mounted Fireplaces [Hedgedoc.Eclair.Ec-Lyon.Fr]
Are You In Search Of Inspiration? Look Up Window Specialists upvc window repair
What NOT To Do In The Purchase Grinding Machines On The Web Industry Gewerbliche Schleifmaschinen Online Kaufen
10 Wrong Answers To Common Asbestos Lung Cancer Louisiana Symptoms Questions: Do You Know The Right Ones? Louisiana Mesothelioma Diagnosis
The 10 Most Scariest Things About Car Crash Attorney car crash attorney (trade-britanica.Trade)
the table beds which we have a year ago had already broken down, it is mostly made up of plastic,.
What Double Glazing Cost Experts Want You To Learn quick double glazing Installation
How To Research Comprehensive Mental Health Assessment Online Comprehensive Mental Health Assessment Online
You'll Never Guess This Pull Out Sleeper Sofa's Tricks pull out sleeper sofa
What Is Door Hinge Replacement And Why Is Everyone Dissing It? composite Door replacement
15 Secretly Funny People Working In Window Replacement Home Window Replacement
3 Reasons Commonly Cited For Why Your Conservatory Repair Cost Isn't Working (And How To Fix It) Conservatory repairs
What's The Job Market For Accident Injury Case Lawyer Professionals? Accident Injury Case Lawyer
Five Killer Quora Answers To Asbestos Lung Cancer Louisiana Risk Asbestos Lung Cancer Louisiana Risk
7 Simple Secrets To Totally Rocking Your Oven And Hobs hobs and ovens
You'll Never Guess This Accident Case Attorney's Tricks Accident Case Attorney
홈타이의 가장 큰 매력은 나만의 편안한 공간에서 주위의 시선을 신경쓰지 않고 프라이빗하게 전문가의 정교하고 전문적인 손길을 누릴 수 있다는 점입니다.
Guide To Accident Injury Settlement Attorney: The Intermediate Guide For Accident Injury Settlement Attorney Accident Injury Settlement Attorney
Mesothelioma Lawsuit Louisiana Tools To Help You Manage Your Everyday Lifethe Only Mesothelioma Lawsuit Louisiana Trick That Should Be Used By Everyone Know Mesothelioma Lawsuit Louisiana (https://Www.haywoodloven.top/)
지식을 공유해 주셔서 정말 감사합니다. 제가 찾은 주제는 정말 훌륭했습니다.
지식을 공유해 주셔서 정말 감사합니다. 제가 찾은 주제는 정말 훌륭했습니다.
The Little-Known Benefits Of Toyota Car Key Lost Toyota Car Key
고객이 머문곳으로 자택, 호텔, 오피스텔 등 대구 출장 마사지는 어디서든 편안한 환경에서 맞춤형 환경 서비스를 제공합니다.
고객이 머문곳으로 자택, 호텔, 오피스텔 등 대구 출장 마사지는 어디서든 편안한 환경에서 맞춤형 환경 서비스를 제공합니다.
Guide To Accident Injury Legal Representation: The Intermediate Guide On Accident Injury Legal Representation Accident Injury Legal Representation; Milsaver.Com,
The 10 Most Scariest Things About Cheap Coffee Maker Online cheap coffee Maker Online
Guide To Sash Window Repair Quotes: The Intermediate Guide To Sash Window Repair Quotes sash window Repair Quotes
14 Companies Doing An Excellent Job At Volvo Car Key Volvo Car Keys Replacement
Why Replacement Key For Toyota Aygo Is So Helpful In COVID-19 Toyota Aygo Key - https://hedgedoc.eclair.ec-lyon.fr/s/irgHCsNhtU,
The 10 Most Scariest Things About Toyota Car Keys Replacement Cost Toyota Car Keys Replacement Cost
What's The Current Job Market For Toyota Spare Key Replacement Professionals Like? Toyota Spare Key Replacement (fakenews.Win)
Five Killer Quora Answers To Conservatory Water Damage conservatory water damage
The 10 Most Terrifying Things About Emergency Vandalism Repair Emergency Vandalism Repair
See What Accident Injury Claim Attorney Tricks The Celebs Are Utilizing Accident Injury Claim Attorney
5 Killer Quora Answers To Personal Injury Attorney Personal Injury Attorney, Milsaver.Com,
Accident Injury Claim Attorney Tips To Relax Your Daily Life Accident Injury Claim Attorney Trick That Everyone Should Be Able To Accident Injury Claim Attorney (https://kanban.xsitepool.tu-freiberg.de/)
Guide To Weight Loss Products Online: The Intermediate Guide Towards Weight Loss Products Online weight loss products online
What You Need To Do On This Diy Window Hinge Repair Fix Loose Window Hinge (https://prosto-robota.com.ua)
As I website possessor I believe the subject material here is rattling fantastic , appreciate it for your efforts.
Think You're Ready To Start Doing Railroad Settlement Pulmonary Fibrosis? Take This Quiz mesothelioma Diagnosis
What's The Current Job Market For Back Door Locks Professionals Like? Back Door Locks
Door Hardware Repair Tools To Ease Your Everyday Lifethe Only Door Hardware Repair Trick That Should Be Used By Everyone Learn Door Hardware repair
9 . What Your Parents Teach You About Accident Insurance Claim Lawyer Accident Insurance Claim Lawyer (rant.li)
See What Upvc Door Panel Specialists Tricks The Celebs Are Using Door Panel Specialists
Accident Injury Attorney Tools To Make Your Daily Life Accident Injury Attorney Trick Every Person Should Learn Accident Injury Attorney
Guide To Accident Lawsuit Representation: The Intermediate Guide For Accident Lawsuit Representation accident Lawsuit Representation
아산출장마사지는 아산 전지역 출장이 가능하고 예약후 원하는 장소에서 바로 관리 받을수 있다는 장점이 있습니다 필요한 대기 없이 깔끔하고 편안한 아산출장마사지 서비스입니다.
Five Killer Quora Answers To Asbestos Lung Cancer Louisiana Risk Asbestos Lung Cancer Louisiana Risk (Www.Altonangelico.Top)
The 10 Scariest Things About Louisiana Lung Cancer Asbestos Exposure louisiana lung cancer asbestos
What's The Job Market For Mesothelioma Louisiana Professionals? Mesothelioma Louisiana
The 10 Scariest Things About Integral Electric Ovens Household appliances
The 10 Scariest Things About Railroad Settlement Leukemia Railroad Settlement Leukemia
You'll Never Be Able To Figure Out This Accident Injury Lawsuit Attorney's Benefits Accident Injury Attorney
What's The Job Market For Cheap Cot Professionals Like? cheap Cots
The 10 Most Terrifying Things About Accident Claim Lawyer Accident Claim Lawyer
The 10 Scariest Things About Private Health Insurance ADHD Assessment Private Health Insurance ADHD Assessment (graph.Org)
The 9 Things Your Parents Teach You About Container 6 Feet Container 6 feet
5 Killer Quora Answers On Accident Injury Lawsuit Attorney Accident Injury Lawsuit Attorney
9 . What Your Parents Taught You About House Key Cutting House Key Cutting
What's The Job Market For Professional Accident Lawyer Professionals Like? professional accident lawyer (Pad.stuve.uni-ulm.de)
You Are Responsible For An Walking Machine With Incline Budget? Twelve Top Ways To Spend Your Money High Incline Treadmill
What's The Fuss About Heavy-Duty Impact Wrench? Schlagschrauber-Shop
A Step-By'-Step Guide To Picking The Right Toyota Replacement Car Keys Toyota Replacement Keys - https://Hackmd.Okfn.de/,
Are You Confident About Doing Sale Bunk Bed? Check This Quiz sale Bunk Beds
감사합니다. 최근 이 주제에 대한 정보를 오랫동안 찾아다녔는데, 당신의 답변이 최고입니다.
감사합니다. 최근 이 주제에 대한 정보를 오랫동안 찾아다녔는데, 당신의 답변이 최고입니다.
Spot on with this write-up, I truly assume this website wants much more consideration. probably be again to read much more, thanks for that info.
See What Best Sofa With Pull-Out Bed Tricks The Celebs Are Using Best Sofa With Pull-Out Bed
9 Things Your Parents Taught You About Undetectable Counterfeit Currency Undetectable counterfeit currency
What's The Current Job Market For Aluminium Window Design Professionals Like? Aluminium Window Design
15 Interesting Facts About Twin Stroller That You Never Knew Twin Strollers
고객이 머문곳으로 자택, 호텔, 오피스텔 등 부산출장 마사지는 어디서든 편안한 환경에서 맞춤형 환경 서비스를 제공합니다.
고객이 머문곳으로 자택, 호텔, 오피스텔 등 부산출장 마사지는 어디서든 편안한 환경에서 맞춤형 환경 서비스를 제공합니다.
See What Cot Bed Wood Tricks The Celebs Are Making Use Of Cot Bed Wood
Responsible For A Volvo Replacement Key Budget? 10 Very Bad Ways To Invest Your Money Volvo Replacement Keys
What Is Fabric Sofas And How To Use It sectional comfy couch
10 Things That Your Family Taught You About Double Glazing Handle Replacement Double Glazing Handle Replacement
Is Your Company Responsible For The Easy-To-Use Planing Machines Budget? 12 Tips On How To Spend Your Money Hobelmaschinen-Rabatte
See What UPVC Door Threshold Repair Tricks The Celebs Are Utilizing UPVC Door Threshold Repair
9 Lessons Your Parents Teach You About Railroad Settlement Stomach Cancer Railroad Settlement Stomach Cancer
7 Things You've Never Learned About Toyota Yaris Key Replacement Toyota Yaris Key Replacement Cost
See What House Rekey Service Tricks The Celebs Are Using House Rekey Service, md.ctdo.de,
Five Killer Quora Answers On Best Fridge Waschmaschine Kaufen
15 Funny People Working Secretly In Key Fob Replacement Toyota Toyota Key
The Mesothelioma Lawyers Louisiana Success Story You'll Never Believe asbestos exposure lung cancer louisiana health risks
See What Robotic Vacuum Cleaners UK Tricks The Celebs Are Utilizing Robotic Vacuum Cleaners Uk
How Fridge Wine Transformed My Life For The Better Fridge for Wine
See What Sash Window Repair And Refurbishment Tricks The Celebs Are Using Sash Window Repair And Refurbishment
What's The Job Market For Window Hinge Repair Near Me Professionals Like? window hinge Repair near Me
5 Killer Quora Answers To Sash Window Renovation Cost Sash Window Renovation Cost
The 10 Most Scariest Things About Window Hinge Repair Company Window Hinge Repair Company
Window Frame Repair Techniques To Simplify Your Daily Life Window Frame Repair Trick Every Individual Should Learn window frame repair
Railroad Settlement Esophageal Cancer Explained In Fewer Than 140 Characters Railroad Settlements
What Do You Think? Heck Is Cot Bed Wood? Solid Wood Cot
What's The Job Market For House Key Cutting Professionals? house key cutting
10 Meetups About Volvo Keys Cut You Should Attend Volvo Key Cutting
10 Things We Love About Oven And Hob ovens And Hob
20 Trailblazers Setting The Standard In Push Pram Sale Prams
A Provocative Rant About Expert House Locksmith Reliable house locksmith
What's The Current Job Market For Professional House Locksmith Professionals Like? Professional House Locksmith (menwiki.men)
You'll Be Unable To Guess Table Mitre Saw's Tricks Table Mitre Saw
10 Quick Tips About Cat Door Assembly reliable cat flap fitter
Five Killer Quora Answers To UPVC Door Seal Repair Upvc Door Seal Repair
9 Lessons Your Parents Taught You About Railroad Settlement Stomach Cancer Railroad Settlement Stomach Cancer (www.Haleema.top)
감사합니다. 최근 이 주제에 대한 정보를 오랫동안 찾아다녔는데, 당신의 답변이 최고입니다.
감사합니다. 최근 이 주제에 대한 정보를 오랫동안 찾아다녔는데, 당신의 답변이 최고입니다.
수원출장마사지 방문마사지 전문 업체로서 수원시 인계동·영통동·매탄동·권선동·세류동·장안동·송죽동·매교동 등 전 지역에서 24시간 언제든 고객님께 맞춤형 마사지를 제공합니다.
What's The Job Market For Handmade Home Furniture Professionals Like? handmade home furniture
What's The Job Market For Small U Shaped Sectional Professionals Like? small u shaped sectional
This is actually the content Now i'm searching for anywhere. Regards for use on your web page, I simply subscribe your blog. They can be a excellent web page. .
the table beds which we have a year ago had already broken down, it is mostly made up of plastic,.
15 Best U Sectional Bloggers You Should Follow Sofa Chase
9 . What Your Parents Taught You About Handmade Sofas UK Sofas UK
블로그 글 정말 좋았어요. 다음 글도 기대할게요. 멋지네요.
블로그 글 정말 좋았어요. 다음 글도 기대할게요. 멋지네요.
getting a masters degree is of course necessary if you want a wage increase and improvement in your career.,
아산출장마사지, 아산출장 전문 테라피스트가 제공하는 고품질 홈·호텔 출장 서비스! 아산출장안마 테크닉으로 깊은 이완을 돕고, 빠른 수원출장 배정으로 즉시 이용 가능합니다.
영등포출장마사지, 영등포출장안마는 고객이 편안함을 느끼는 공간으로 전문 마사지사가 직접 방문해 마사지를 제공하는 24시 영등포출장 서비스입니다. 선입금 없는 후불제로 안심하고 이용할수 있습니다.
Door Frame Hinge's History History Of Door Frame Hinge emergency door Hinge repair [www.Supergame.one]
Five Killer Quora Answers On Twenty Foot Container Twenty Foot Container
UPVC Door Company Tools To Make Your Everyday Lifethe Only UPVC Door Company Trick That Should Be Used By Everyone Learn UPVC Door Company
This Story Behind Window Hinge Repairs Will Haunt You For The Rest Of Your Life! affordable window hinge Repairs
The 10 Most Scariest Things About Cheap Coffee Machine UK Cheap Coffee Machine uk
7 Helpful Tricks To Making The Maximum Use Of Your Window Hinge Restoration window hinge restoration services
Guide To 45ft Shipping Container Rental: The Intermediate Guide On 45ft Shipping Container Rental 45Ft shipping container rental
The Best All Terrain Prams Tricks To Make A Difference In Your Life Best All Terrain Prams
You'll Be Unable To Guess Sash Windows Repair And Servicing's Secrets Sash Windows Repair And Servicing
Why The Biggest "Myths" Concerning Adjustable Office Desks Online Might Be True Compra Convertidores De Escritorio Ajustables Online
Nine Things That Your Parent Taught You About Planing Machines Price Planing Machines Price
10 Things That Your Family Teach You About Buy Counterfeit Euros Buy Counterfeit Euros
See What Auto Smart Key Tricks The Celebs Are Making Use Of auto smart key
What's The Current Job Market For Disabled Scooters Near Me Professionals Like? disabled scooters Near me
Why You Should Focus On Making Improvements To Shipping Container 45ft 45ft shipping containers
The No. Question That Everyone In Best Way To Get Polish License Must Know How To Answer jazda Bez prawa Jazdy
10 Things You Learned In Preschool That'll Help You Understand Hungarian Driving License Registration getting a Hungarian Driving license
What Is The Future Of Professional Planing Machines Be Like In 100 Years? Hobelmaschinen Mit Garantie
Say "Yes" To These 5 U Shaped Sectional Tips Sofa Chaise Lounge
You'll Never Guess This High Bed With Slide's Tricks high bed With slide
10 Facts About Convertible Cot Bed That Will Instantly Get You Into A Great Mood Convertible Cot Bed With Mattress
Swiss Road Regulations Tools To Help You Manage Your Daily Life Swiss Road Regulations Trick That Every Person Must Be Able To Swiss road regulations
Private ADHD Assessment Adult Tools To Streamline Your Daily Life Private ADHD Assessment Adult Trick That Everybody Should Know Private ADHD Assessment Adult
Guide To Smart Car Key Fob Replacement: The Intermediate Guide Towards Smart Car Key Fob Replacement Smart Car Key Fob
See What Buy 1kg Coffee Beans Tricks The Celebs Are Using buy 1kg Coffee beans
20 Trailblazers Leading The Way In Private Psychiatrist Psychiatrists Private
Guide To Foldable Lightweight Wheelchair: The Intermediate Guide For Foldable Lightweight Wheelchair Foldable Lightweight Wheelchair
Guide To Accident Settlement Lawyer: The Intermediate Guide On Accident Settlement Lawyer Accident Settlement Lawyer, https://pattern-wiki.win/wiki/10_Signs_To_Watch_For_To_Look_For_A_New_Accident_Injury_Legal_Representation,
The 9 Things Your Parents Teach You About Patio Door Repairs Near Me Patio Door Repairs Near Me
The 10 Most Scariest Things About 65-inch LG Smart TV Beamer Mit WLAN Und Bluetooth
Private ADHD Explained In Fewer Than 140 Characters Adhd Diagnosis
What's The Current Job Market For Collapsible Power Wheelchair Professionals Like? Collapsible Power Wheelchair
Five Reasons To Join An Online Auto Key Duplication Buyer And 5 Reasons Why You Shouldn't online auto key
Buy Height Adjustable Table Online: What's The Only Thing Nobody Is Discussing Compra Productos ErgonóMicos De Oficina Escritorios
Accident Injury Settlement Attorney Tools To Make Your Everyday Lifethe Only Accident Injury Settlement Attorney Trick That Everyone Should Be Able To Accident injury settlement Attorney
What's The Job Market For Childrens Bunk Bed With Desk Professionals? childrens Bunk Bed with desk
5 Killer Quora Answers To Affordable Glazier Affordable Glazier
See What Ovens Integrated Tricks The Celebs Are Using Ovens integrated
Learn To Communicate Bosch GHP 5-75 X Professional To Your Boss Kränzle Hochdruckreiniger Preisvergleich
You'll Be Unable To Guess Built In Appliances's Tricks Built In Appliances
5 Freezers For Sale Projects For Every Budget WäSchetrockner Versandkostenfrei
15 Lessons Your Boss Wished You'd Known About Top Rated Washer Dryer Waschtrockner-Sets kaufen (stroyrem-master.ru)
15 Terms Everyone Involved In Find A Psychiatrist UK Industry Should Know Private Psychiatrist Assessment Near Me (Clinfowiki.Win)
The 10 Scariest Things About Pomegranate Extract Vs Urolithin A Supplement Pomegranate Extract vs Urolithin A Supplement
How To Save Money On Acer DLP Projector Full HD Beamer Für Tageslicht
You'll Never Guess This Delonghi Coffee Machine With Grinder's Tricks Delonghi Coffee Machine With Grinder
9 . What Your Parents Taught You About Handmade Seat Handmade Seat
Watch This: How Cisco 730 On-Ear Bluetooth Headset Is Taking Over And How To Respond Benq Heimkino Beamer (directorytome.com)
15 Tips Your Boss Wants You To Know About Fridges You Knew About Fridges Cheap Fridges Online
Guide To Smart Car Key Fob Replacement: The Intermediate Guide To Smart Car Key Fob Replacement Smart Car Key Fob
What's The Job Market For Kids Bunk Bed Professionals Like? kids bunk Bed
See What Bariatric Wheelchair Electric Tricks The Celebs Are Using Bariatric Wheelchair Electric
Guide To Fitted Ovens And Hobs: The Intermediate Guide Towards Fitted Ovens And Hobs fitted ovens and hobs
You'll Never Guess This What Is The Best French Door Refrigerator's Secrets what is the best french door refrigerator
10 Methods To Build Your Where Can I Get A Kia Key Made Empire Kia Keys
What's The Current Job Market For Mazda Spare Key Cost Professionals? Mazda Spare Key Cost
What's The Current Job Market For Rubber Door Seals Professionals Like? Rubber Door Seals (Scientific-Programs.Science)
10 Meetups About Cot Bed You Should Attend recommended Cribs
The 10 Scariest Things About Baby Cot Bed Baby Cot Bed
This Is The Ugly The Truth About Bedside Cot For Sleeping Arrangements white cot bed With drawer, www.ludikarus.com,
Window Handle Replacement Service Techniques To Simplify Your Daily Life Window Handle Replacement Service Trick That Everyone Should Be Able To Window Handle Replacement Service
10 Things That Your Family Taught You About Seat Cordoba Key Replacement seat cordoba key replacement, nerdgaming.science,
What's The Current Job Market For Best Sash Window Repair Contractors Professionals? Best Sash Window Repair Contractors
You'll Never Guess This Baby Co Sleeper Crib's Tricks Baby Co Sleeper Crib (To-Portal.Com)
5 Killer Quora Answers To Robot Vacuum Cleaner With Mop Self Empty Base Robot vacuum cleaner With mop self empty base
House Lock And Key Services Tips To Relax Your Daily Life House Lock And Key Services Trick That Every Person Must Be Able To House lock and key services
See What Accident Injury Legal Advice Tricks The Celebs Are Utilizing Accident Injury Legal Advice
15 Gifts For The Danish Driving Rules Lover In Your Life HjæLp Til Dansk Kørekort
What Is The Reason? Patio Doors Repairs Is Fast Becoming The Hot Trend For 2024 Patio Door Panel Repair
See What 6 Foot Shipping Container Tricks The Celebs Are Making Use Of 6 foot shipping container
Guide To 24 Inch Bariatric Transport Wheelchair: The Intermediate Guide For 24 Inch Bariatric Transport Wheelchair 24 inch bariatric transport wheelchair
One Mini Key Replacement Success Story You'll Never Be Able To Mini Key Replacement Cost
What's The Current Job Market For Broken Window Hinge Repair Professionals Like? Broken Window Hinge Repair
7 Practical Tips For Making The Most Of Your Treadmill With Incline Portable Treadmill With Incline
What Is Weather Seal Replacement's History? History Of Weather Seal Replacement Window Gasket Seals (hedgedoc.eclair.ec-lyon.fr)
How To Beat Your Boss With Private Psychiatric Assessment Private Psychiatry clinic
See What Auto Accident Injury Lawyer Tricks The Celebs Are Making Use Of Auto Accident Injury Lawyer (https://mohamed-reeves.hubstack.net/10-wrong-answers-to-common-injury-compensation-questions-do-you-know-the-right-ones)
10 Things That Your Family Teach You About Accident Injury Compensation Claim Lawyer Accident Injury Compensation Claim Lawyer
ADHD Private Assessment UK Tools To Streamline Your Everyday Lifethe Only ADHD Private Assessment UK Trick That Every Person Must Know adhd private assessment uk
Speak "Yes" To These 5 Buy A German Driver's License Tips füHrerschein Express
10 Tips For Quickly Getting BenQ Home Theater Projector LG Smart TV 65 Zoll
10 Apps To Help Manage Your Cheap Cotbeds best baby Travel cot
What's The Current Job Market For Private ADHD Assesment Professionals Like? Private ADHD Assesment
5 Heavy Demolition Hammer Price Lessons From The Professionals werkzeuge für profis online shop
Five Killer Quora Answers On UPVC Door Water Leak Repair UPVC Door Water Leak Repair
14 Cartoons About Drill Test Which Will Brighten Your Day Werkzeug Online Kaufen
15 Unexpected Facts About Electric Drill You Didn't Know Drill Special Offer
See What L Couch Tricks The Celebs Are Making Use Of L Couch
See What Best Robotic Hoover Tricks The Celebs Are Utilizing best robotic hoover
Best Robot Hoover Tools To Make Your Daily Life Best Robot Hoover Trick That Should Be Used By Everyone Be Able To best robot hoover (https://perry-burgess-2.technetbloggers.de/everything-you-need-to-learn-about-robotic-vacuum)
What U Shape Sofa Experts Want You To Learn couch with lounger (https://Telegra.ph)
The 10 Scariest Things About BMW Key Fob Replacement BMW Key Fob Replacement
The No. One Question That Everyone Working In Self-contained Induction Hob Test Should Be Able To Answer Induktionskochfeld Rahmenlos Angebot (Securityholes.science)
A New Trend In Planing Machines Discounts Hobelmaschinen Zum Besten Preis
Five Killer Quora Answers On Pushchair Off Road Pushchair Off Road
The 10 Most Scariest Things About Bedside Cot For Peaceful Nights Bedside Cot For Peaceful Nights
7 Useful Tips For Making The Most Out Of Your Buying A Driving License Experiences FüHrerschein Ohne PrüFung Legal - Voovixtv.Com -
Kids Bed With Desk Underneath Tools To Improve Your Daily Lifethe One Kids Bed With Desk Underneath Trick That Every Person Should Learn Kids Bed With Desk
You'll Never Guess This Suzuki Alto Key Fob's Tricks Suzuki Alto Key Fob
11 Methods To Redesign Completely Your Purchase Cordless Power Tools Sortiment An Akku-Elektrowerkzeugen
This Is The History Of Compressor Purchase In 10 Milestones Online-Kompressorvertrieb
5 Reasons To Consider Being An Online Best Value Washing Machines Business And 5 Reasons You Shouldn't Waschmaschinen Kaufen
Guide To Vauxhall Vivaro Replacement Key: The Intermediate Guide On Vauxhall Vivaro Replacement Key Vauxhall vivaro replacement Key
10 Car Key Replacement Vauxhall That Are Unexpected vauxhall car Key
The 10 Scariest Things About Nescafe Gusto Dolce Nescafe Gusto dolce
The Best Way To Explain French Fridge Freezer To Your Boss French freezer
5 Laws That Anyone Working In Bariatric Wheelchair Should Know Bariatric Wheelchair With Deep Seat
Don't Forget Dewalt Tool: 10 Reasons Why You Do Not Need It Dewalt Products
Say "Yes" To These 5 Buying Driving License In Finland Tips Suomen Ajokortin Ostaminen
A Look In The Secrets Of How To Get A Mental Health Diagnosis UK Private Private Mental Health Diagnosis (https://doc.adminforge.de)
The 10 Scariest Things About MItolyn Side Effects Mitolyn Side Effects
14 Businesses Doing An Amazing Job At Citroen Keys citroen ds3 key Programming
Buy Small Grinders Online: What's The Only Thing Nobody Is Talking About Beste Schleifmaschinen Im Angebot
Your Family Will Thank You For Having This Restore UPVC Doors UPVC Door Restoration
How To Make An Amazing Instagram Video About Portable Washer Dryer Waschtrockner Online kaufen
What's The Current Job Market For Honda Jazz Car Key Replacement Professionals? Honda jazz car Key replacement
4 Wheel All Terrain Pushchair Tips From The Top In The Industry Compact All Terrain Stroller
Residential Door Locksmith Techniques To Simplify Your Daily Lifethe One Residential Door Locksmith Trick That Every Person Must Be Able To Residential Door Locksmith
You'll Be Unable To Guess Unique Handmade Reclining Sofa's Tricks Sofa
Refurbished Sage Coffee Machines Tools To Help You Manage Your Daily Lifethe One Refurbished Sage Coffee Machines Trick Every Person Should Know Refurbished Sage Coffee Machines (duus-Warming-2.thoughtlanes.net)
"Ask Me Anything," 10 Answers To Your Questions About Buy Yorkshire Mix Puppies Yorkies
See What Compact Stoves Online Tricks The Celebs Are Using compact Stoves online
See What Restore UPVC Doors Tricks The Celebs Are Making Use Of Restore UPVC Doors
10 4-Wheel Walker Tips All Experts Recommend Foldable 4-Wheel Walker
Guide To Bean To Cup Coffee Maker: The Intermediate Guide In Bean To Cup Coffee Maker Bean To Cup Coffee Maker
The Reason Behind Double Glazed Window Repairs Is The Most Popular Topic In 2024 Window Repair Service
Modern House Locksmith Tools To Ease Your Daily Lifethe One Modern House Locksmith Trick That Everyone Should Know Modern House Locksmith
Guide To Volvo Approved Locksmith Near Me: The Intermediate Guide The Steps To Volvo Approved Locksmith Near Me volvo approved locksmith near Me
The Leading Reasons Why People Perform Well On The Buy A Real Driving License Industry füHrerschein Kaufen Deutschland (pad.geolab.space)
See What Cat Door Experts Tricks The Celebs Are Utilizing cat door expert
How To Make An Amazing Instagram Video About Cotbeds recommended cribs
You'll Never Be Able To Figure Out This Fix Stuck Window Hinge's Benefits fix stuck window hinge (https://iskustva.net)
Guide To Expert Accident Lawyer: The Intermediate Guide In Expert Accident Lawyer Expert Accident Lawyer
Local Sash Window Restoration Experts Tools To Improve Your Everyday Lifethe Only Local Sash Window Restoration Experts Trick That Every Person Must Know Local Sash Window Restoration Experts
Fixing Conservatory Issues: What's The Only Thing Nobody Is Talking About Window Latch Repair (Hatch-Reeves.Thoughtlanes.Net)
9 Lessons Your Parents Teach You About Adults Bunk Beds Adults Bunk Beds
You'll Never Be Able To Figure Out This Peugeot Spare Key's Benefits peugeot Spare key
The Hidden Secrets Of Foldable Wheelchair Light Foldable Wheelchair
What's The Job Market For Tilt And Turn Mechanism Repair Professionals Like? Tilt And Turn Mechanism Repair (Https://Hackmd.Okfn.De)
9 Signs That You're A Add Test For Adults Expert Add Test For Adults Online
The 10 Scariest Things About Draft Seals Draft Seals
See What Cordless Circular Saw With Battery And Charger Tricks The Celebs Are Using Cordless Circular Saw With Battery And Charger
How To Explain Psychiatrist To Your Grandparents Private Psychiatrist Cost
9 Signs You're A Small Prams For Newborns Expert fabric
Electric Sweepers Tips That Will Change Your Life Motorisierte Kehrmaschinen
Guide To Purchasing Medication Online: The Intermediate Guide In Purchasing Medication Online Purchasing Medication Online
9 . What Your Parents Taught You About Accident Injury Lawsuit Representation Accident Injury Lawsuit Representation
Induction Hob Set Offer Tips From The Top In The Industry Backofen Einbau 60 Cm Angebot; timeoftheworld.date,
10 Things That Your Family Taught You About Twin Travel System Twin Travel System
7 Tricks To Help Make The The Most Of Your Buy A Top-Loading Washing Machine At A Great Price frontlader Waschmaschine Vergleich
Guide To Robotic Vacuum Cleaner Self Emptying: The Intermediate Guide For Robotic Vacuum Cleaner Self Emptying Robotic Vacuum Cleaner Self Emptying
10 Inspirational Images Of U Sectionals Chaise Lounge Couch
The No. 1 Question Everyone Working In Top Grinding Machines To Buy Online Must Know How To Answer Schleifmaschinen Im Web (Nance-Berger-3.Mdwrite.Net)
An In-Depth Look Into The Future What's The All-Weather Tire Price Comparison Industry Look Like In 10 Years? Bridgestone Turanza 6 Preisvergleich
12 Facts About Dolce Gusto Coffee That Will Make You Think Twice About The Cooler. Cooler Compact
The 10 Scariest Things About Accident Legal Counsel Accident Legal Counsel
15 Presents For The Weather Stripping Lover In Your Life door Weather Stripping
What's The Job Market For New Pallets For Sale Professionals? new pallets For sale
Ford Keyless Fob Replacement Tools To Ease Your Daily Life Ford Keyless Fob Replacement Trick That Every Person Must Learn Ford Keyless Fob Replacement
What's The Current Job Market For Folding Lightweight Electric Wheelchair Professionals? folding lightweight electric wheelchair
10 Things That Your Family Teach You About Double Pushchair Sale Double Pushchair Sale
Private Online Psychiatrist Tools To Improve Your Daily Life Private Online Psychiatrist Trick That Every Person Must Know Private Online Psychiatrist
5 Killer Quora Answers On House Security Locksmith House Security Locksmith
How Independent Built-In Oven Changed My Life For The Better Frontlader 8 Kg Energieeffizienzklasse A
What's The Current Job Market For Replacement Hyundai Key Fob Professionals? Replacement Hyundai Key Fob
For Whom Is Integrated Electric Oven And Why You Should Take A Look integrated electric oven And hob
Wholesale Bulk Coffee Bean Prices Tips To Relax Your Everyday Lifethe Only Wholesale Bulk Coffee Bean Prices Trick That Every Person Should Know wholesale bulk Coffee bean Prices
5 Killer Quora Answers On Psychiatrist Private Psychiatrist Private
The Three Greatest Moments In Restoring Conservatory History Window lock maintenance
11 Methods To Refresh Your American Fridge Freezer Deals waschtrockner schmal Preis; http://35.168.82.226:3000/waschmaschine-8kg-Test9971,
Cordless Hand Saw Techniques To Simplify Your Daily Life Cordless Hand Saw Technique Every Person Needs To Learn Cordless hand saw
This Most Common Coffee Bean Machine Debate It's Not As Black And White As You Think Coffee Bean Machines
9 . What Your Parents Teach You About Affordable Window Doctor Affordable Window Doctor
Twin Pushchairs Techniques To Simplify Your Everyday Lifethe Only Twin Pushchairs Trick That Should Be Used By Everyone Be Able To twin pushchair
Solutions To The Problems Of Pram Vs Pushchair Carriage
Aluminum Window Handle Replacement Tools To Help You Manage Your Daily Life Aluminum Window Handle Replacement Trick That Every Person Should Be Able To aluminum window handle Replacement (Https://moparwiki.win/)
10 Things That Your Family Teach You About Accident Injury Lawsuit Representation Accident injury lawsuit representation
The 10 Most Scariest Things About Interior Lighting UK Interior Lighting
See What Bunk Bed Adult Tricks The Celebs Are Utilizing bunk Bed adult
Five Killer Quora Answers To Bedside Cot For Contemporary Design Bedside Cot For Contemporary Design - https://md.chaosdorf.de/0iDg0fiSQyyozO4mNxKf_g -
What's The Reason? Buy A2 Driver's License Online Is Everywhere This Year Führerschein Digital Kaufen
15 Reasons Not To Be Ignoring Best Cot tots And cots
5 Killer Quora Answers To Door Insulation Door Insulation
Broken Window Hinge Replacement Tips From The Most Successful In The Business Window Hinges
What's The Job Market For Old Window Handle Replacement Professionals? Old Window Handle Replacement
The 10 Most Scariest Things About Legal Advice For Accidents Legal Advice For Accidents (hackmd.okfn.de)
The 10 Most Terrifying Things About Replacement Porsche Key Fob Porsche Key Fob
The Top Reasons Why People Succeed In The Best Online Store For Weight Loss Drugs Industry weight loss Drugs online
You'll Never Guess This Land Rover Key Replacement's Secrets land rover key replacement, https://graph.org,
The Advanced Guide To Couches best places to buy Couches
See What Bedside Crib For Small Spaces Tricks The Celebs Are Making Use Of bedside crib for small spaces
9 Lessons Your Parents Taught You About Sash Window Repairman In My Area Sash Window Repairman In My Area
Responsible For An Kia Sportage Key Budget? 12 Best Ways To Spend Your Money Kia Sportage Key Fob (https://pad.karuka.tech)
See What Accident Injury Compensation Attorney Tricks The Celebs Are Using accident Injury compensation attorney
An Adventure Back In Time The Conversations People Had About Cordless Machine Set Prices 20 Years Ago Günstiges Akku-Maschinenset
You'll Be Unable To Guess Trusted House Locksmith's Benefits Trusted House Locksmith
See What Accident Legal Counsel Tricks The Celebs Are Utilizing Accident Legal Counsel - Hedgedoc.eclair.ec-lyon.fr -
5 Killer Quora Answers On Dual Boiler Espresso Machine Dual Boiler Espresso Machine
10 Easy Ways To Figure Out Your Planing Machines For Furniture Hobelmaschinen-Auswahl
5 Killer Quora Answers On Subaru Replacement Fob subaru replacement fob
It's Time To Extend Your Versatile Electric Treadmills Options Electric Treadmill Comparison
Speak "Yes" To These 5 Learn To Drive UK Tips Practical Driving Test
Five Tools Everybody In The Online ADHD Testing Industry Should Be Using Adult ADHD Test Online
5 Killer Quora Answers On Affordable Wooden Pallets Affordable Wooden Pallets [king-wifi.win]
9 . What Your Parents Teach You About Programmable Sage Coffee Machines Programmable Sage Coffee Machines (www.folkd.com)
10 Places To Find Cots For Babies cots offers
Five Killer Quora Answers On User-Friendly Electric Treadmills User-Friendly Electric Treadmills
Will Bed With Desk Ever Be The King Of The World? Double Bed Bunk Bed With Desk
The 10 Scariest Things About Legal Advice For Accidents Legal Advice For Accidents
Test For ADHD Tools To Make Your Everyday Lifethe Only Test For ADHD Technique Every Person Needs To Know Test For ADHD
See What Accident Injury Claim Attorney Tricks The Celebs Are Using accident injury claim attorney
20 Things You Should Know About Sectional Sofa Pull Out Bed Pull Out Beds (https://doc.aquilenet.fr/CZmJbn97RmWzTjHrkh7ZWA)
The 10 Most Dismal Couch Cheap Failures Of All Time Could Have Been Prevented couches
See What Repair Broken Tilt And Turn Windows Tricks The Celebs Are Utilizing repair broken tilt and turn windows
Why Standing Compressor 50L Still Matters In 2024 Trockenbauschleifer Mit Staubsauger Set GüN
15 Things You've Never Known About Inverter Welding Machine Test mig mag schweißgerät set angebot
The 10 Most Scariest Things About Study Bunk Study Bunk
Nine Things That Your Parent Teach You About Repairing Old Tilt And Turn Windows Repairing Old Tilt And Turn Windows
You'll Never Be Able To Figure Out This Broken Window Hinge Repair's Secrets Broken Window Hinge Repair
Are You Making The Most From Your Sofa? Handmade Leather Sofa
What You Can Use A Weekly Buy Professional Pressure Washer Project Can Change Your Life Hochdruckreiniger FüR Den Hausgebrauch - Https://Articlescad.Com/10-Factors-To-Know-About-Pressure-Washer-Offers-You-Didnt-Learn-In-The-Classroom-55995.Html -
10 Meetups About French Door Fridges On Sale You Should Attend French Door Fridge Sale
How To Explain Michelin Alpin 6 205 55 R16 To Your Mom michelin alpin 6 205/55 r16 (https://pad.Geolab.space/)
5 Clarifications Regarding Land Rover Key Replacement land rover Key replacement near me
You'll Never Be Able To Figure Out This Suzuki Swift Remote Key Replacement's Benefits Suzuki Swift Remote Key Replacement
Guide To Best Place To Buy Counterfeit Money: The Intermediate Guide Towards Best Place To Buy Counterfeit Money Best Place To Buy Counterfeit Money, Https://bigdatahiring.com/,
You'll Be Unable To Guess Replacement Car Keys Ford's Benefits Replacement Car Keys Ford
Five Killer Quora Answers To Fiat 500 Replacement Key Cost Fiat 500 Keys
Why You Should Concentrate On The Improvement Of Cheap Cotbeds Top Rated Cots
16 Must-Follow Instagram Pages For Mental Health Test UK-Related Businesses Book A Mental Health Assessment
14 Common Misconceptions About Honda Car Key Replacement Honda Car Key Replacement Cost (Md.Un-hack-Bar.de)
15 Best Documentaries About Window Hinge Replacement Window Hinge Replacement Cost
The Top Reasons Why People Succeed On The Couches Industry best reclining couch
10 Meetups About BMW Key You Should Attend BMW Key Repair (123-directory.com)
The 10 Most Terrifying Things About Lost Kia Car Key Lost Kia Car Key
8 Tips To Up Your Goethe B1 Certificate Cost Game B1 Deutsch Zertifikat Goethe-Zertifikat Online Kaufen
Ten Powertools That Really Improve Your Life powertools
See What Accident Injury Law Firm Tricks The Celebs Are Using Accident Injury Law Firm
What's The Current Job Market For Legal Representation For Accidents Professionals? Legal Representation For Accidents
Guide To Accident Case Attorney: The Intermediate Guide To Accident Case Attorney Accident Case Attorney
What's The Current Job Market For Saab Key Professionals? saab key Fob
5 Qualities That People Are Looking For In Every Buy A Compressor For The Garage Druckluft Kompressor 10 Bar
You'll Never Guess This Motor Vehicle Accident Attorney's Secrets Motor Vehicle Accident Attorney, https://earthloveandmagic.com/activity/p/1639900/,
You'll Never Be Able To Figure Out This Upvc Panel Maintenance's Tricks UPVC Panel Maintenance
Guide To Integrated Oven Sizes: The Intermediate Guide To Integrated Oven Sizes integrated oven sizes
See What Baby Bedside Sleeper Tricks The Celebs Are Utilizing Baby Bedside Sleeper
9 . What Your Parents Taught You About Baby Wooden Cot baby wooden cot
20 Reasons To Believe Mobile Ramps For Wheelchairs Will Never Be Forgotten Ramp For Wheelchair
15 Presents For Your Price Of A Fridge Lover In Your Life Fridge Price
How Much Can Portable Compressor Buy Experts Make? Kompressor Online Kaufen
5 Laws To Help The Tandem Stroller Industry Tandem Strollers (https://isowindows.net/user/garagesister1)
Five Killer Quora Answers On Electric Oven & Hob oven & Hob
7 Essential Tips For Making The Most Of Your Private Bipolar Diagnosis UK Psychiatrist Near Me Private Practice (Https://Hackmd.Okfn.De)
Why Window Hinge Restoration Is Fast Increasing To Be The Most Popular Trend In 2024 Window Hinge Restoration Services (King-Wifi.Win)
The 10 Scariest Things About Conservatory Roof Repair conservatory Roof repair
What's The Job Market For UPVC Door Water Leak Repair Professionals Like? UPVC Door Water Leak Repair
5 Killer Quora Answers On Sash Window Repair Cost sash window repair cost
5 Bosch Tassimo Projects That Work For Any Budget Bosch Tassimo Coffee Maker (Https://6.k1668.cn/)
See What Land Rover Discovery Sport Key Replacement Cost Tricks The Celebs Are Using Land Rover Discovery Sport Key Replacement Cost
Guide To Robot Cleaner Vacuum And Mop: The Intermediate Guide To Robot Cleaner Vacuum And Mop Robot Cleaner Vacuum And Mop
Espresso Machine With Dual Shot Tools To Streamline Your Daily Life Espresso Machine With Dual Shot Technique Every Person Needs To Know espresso machine with Dual shot
A Relevant Rant About ADHD Test Adult Online Online adhd test for Adults
"The Bypass The TestDaF Exam Awards: The Most Stunning, Funniest, And The Most Bizarre Things We've Seen Testdaf Zertifikat Ohne PrüFung Online Beantragen
A Good Rant About Coffee Beans 1kg UK 1kg Bag Of Coffee Beans
Full Mental Health Assessment Tools To Ease Your Daily Lifethe One Full Mental Health Assessment Trick Every Individual Should Be Able To Full Mental Health Assessment (discoveringalifeyoulove.com)
We've Had Enough! 15 Things About Buy European Driving License Online We're Sick Of Hearing RegisztráLt Vezetői Engedély Vásárlása
You'll Never Guess This Precision Mitre Saw's Benefits Precision Mitre Saw
What's The Reason Nobody Is Interested In Sofa U Shape u-shaped Sofa
How To Explain L Couches To Your Grandparents L Sectional Couch
14 Cartoons About Goethe Certificate Which Will Brighten Your Day sprachzertifikat Kaufen - md.Ctdo.de,
Built In Oven Uk Techniques To Simplify Your Daily Life Built In Oven Uk Trick That Everyone Should Learn built in oven uk (output.Jsbin.com)
15 Shocking Facts About Planer Combination Device Profi Werkzeug Online Shop
The 10 Most Terrifying Things About Compact Folding Wheelchair Compact Folding Wheelchair - Https://Md.Chaosdorf.De/ -
Learn About Italian Driving License Trusted Seller While You Work From At Home Patente Di Guida Online
11 "Faux Pas" That Are Actually Acceptable To Use With Your Bang & Olufsen Headphone Deal Gaming Smartphone Test (Rentry.Co)
Updating Conservatory Tools To Ease Your Daily Lifethe One Updating Conservatory Trick That Everybody Should Be Able To Updating Conservatory
9 Lessons Your Parents Teach You About Grinder Cordless Grinder Cordless
The Reasons Buy A Freestanding Refrigerator Is Everywhere This Year Kühlschrank Mit 0 Grad Zone Test
A Provocative Remark About Refrigerator With Ice Cube Dispenser Offer Kühl-Gefrier-Kombination Kaufen
The Worst Advice We've Heard About Buy Sweepers Online Kehrmaschinen Für Betriebe; Http://bbs.51pinzhi.cn/home.php?mod=space&uid=7554719,
20 Trailblazers Lead The Way In Folding Electric Wheelchair Auto folding Electric wheelchair
Why Newborn Prams And Pushchairs Is Fast Increasing To Be The Most Popular Trend In 2024 double pram Pushchair (https://hack.allmende.io)
The Time Has Come To Expand Your Robot Floor Cleaner Options best Automatic vacuum cleaner
The 10 Scariest Things About Upvc Panel Restoration upvc Panel restoration
The Reason Why Everyone Is Talking About Summer Tires 205 55 R16 Right Now Pirelli Cinturato All Season SF2 GüNstig
The 10 Scariest Things About Panel Repair Experts Panel Repair Experts (Eliasen-thomsen-2.Blogbright.net)
How Ignition Repair Services Influenced My Life For The Better Car Ignition Repair Services
15 Surprising Facts About Suzuki Keys Suzuki Keys Replacement
The 9 Things Your Parents Teach You About 1kg Coffee Beans Price 1Kg Coffee Beans Price
5 Killer Quora Answers On Side By Side Double Stroller Side By Side Double Stroller
Guide To Auto Folding Mobility Scooters: The Intermediate Guide Towards Auto Folding Mobility Scooters auto Folding mobility scooters (https://pads.jeito.nl)
An Adventure Back In Time How People Talked About Shop For Planing Machines 20 Years Ago Hobelmaschinen-Preise (Diego-Maradona.Com.Az)
A Brief History Of The Evolution Of Volvo Key Replacement Volvo Keys
Guide To Mazda Lost Key Replacement: The Intermediate Guide For Mazda Lost Key Replacement Mazda Lost Key Replacement
Guide To Accident Case Attorney: The Intermediate Guide In Accident Case Attorney accident case Attorney
The 10 Most Terrifying Things About Window Handle Cover Replacement Window Handle Cover Replacement
Guide To Fireplace Electric With Mantel: The Intermediate Guide For Fireplace Electric With Mantel Fireplace Electric With Mantel
This Is How Volkswagen Lost Key Will Look Like In 10 Years' Time Lost volkswagen Key
7 Things About Electric Fireplaces With Mantle You'll Kick Yourself For Not Knowing Electric fireplace With mantle
Damaged Window Hinge Repair Tools To Make Your Day-To-Day Life Window Hinge Repair Tools
Mobility Scooter Shops Near Me Techniques To Simplify Your Daily Life Mobility Scooter Shops Near Me Trick Every Individual Should Know mobility scooter shops near me
The Unknown Benefits Of Lexus Key Replace Lexus Key Fob
Five Patio Doors Repairs Lessons From Professionals Patio Door Replacement
5 Killer Quora Answers On 22 Inch Seat Wheelchair 22 Inch Seat Wheelchair
5 Killer Quora Answers To How Much Is A Mental Health Evaluation how much is a mental health evaluation
The 10 Most Terrifying Things About Sliding Window Handle Replacement Sliding Window Handle Replacement
See What Door Panel Refurbishing Tricks The Celebs Are Making Use Of Door panel Refurbishing
Why You Should Focus On Making Improvements To Buy Valid European Driver's License comprar carnet De conducir español online (Securityholes.science)
The 10 Most Scariest Things About Toyota Car Keys Replacement Cost Toyota Car Keys Replacement Cost
You'll Never Be Able To Figure Out This UPVC Door Repair Professional's Tricks UPVC Door Repair Professional
The 10 Most Scariest Things About Failed Double Glazing failed Double glazing
See What Fiat 500 Electric Key Tricks The Celebs Are Utilizing Fiat 500 Electric Key
Guide To Bedside Cot For Versatile Use: The Intermediate Guide On Bedside Cot For Versatile Use Bedside Cot For Versatile Use
It's True That The Most Common Spanish Driving License Debate Could Be As Black And White As You May Think Carne De Conducir Europea Barata En EspañA
5 Things That Everyone Is Misinformed About On The Subject Of French Driving License Application permis de conduire français Abordable
20 Tools That Will Make You Better At Buy Fakes beste webseite Für falschgeld
Automatic Vacuum And Mop Techniques To Simplify Your Daily Lifethe One Automatic Vacuum And Mop Trick That Should Be Used By Everyone Know Automatic Vacuum
The 10 Most Scariest Things About Failed Double Glazing Failed Double Glazing
You'll Never Guess This Replacement Key For Hyundai I30's Tricks replacement key for hyundai i30
Bedside Cot For Modern Nursery Tips From The Top In The Business Cot Bed With Drawers
10 Unexpected Buy Robot Vacuum Tips Robot Vacuum Cleaner
It's The Double Prams Case Study You'll Never Forget Double Pram For Twins
15 American Fridge Sale Benefits Everyone Should Be Able To Washing Machine Test Winner Price-Performance Ratio 2025
9 . What Your Parents Taught You About Robot Vacuum Self Cleaning Robot Vacuum Self Cleaning
10 Things We Are Hating About Handle Grinder Handheld Grinder (Https://Notes.Io/EwYXn)
The Most Convincing Proof That You Need Buy A Cheap Chest Freezer Gefriertruhe Groß Preis
Guide To Battery Circular Saws: The Intermediate Guide Towards Battery Circular Saws Battery Circular Saws
How To Create An Awesome Instagram Video About Mitsubishi Key Replacement mitsubishi key Replacement near me - Posteezy.Com,
Five Killer Quora Answers On Seat ARONA Key Replacement seat arona key Replacement
What Is Continental WinterContact TS 870? History Of Continental WinterContact TS 870 Michelin Crossclimate Preis
Ten Startups That Are Set To Change The Counter Display Case Industry For The Better speisenwaermer Gastronomie
Nine Things That Your Parent Taught You About Double Bunk Beds For Adults UK Bunk Beds for adults uk
Five Killer Quora Answers To Mitre Saws For Sale Mitre Saws For Sale
Sash Window Restoration Near Me Tips To Relax Your Daily Life Sash Window Restoration Near Me Trick That Everyone Should Know Sash Window Restoration Near Me
Could Professional Pressure Washer Be The Answer For 2024's Challenges? kärcher hd 5/15 c plus
What Is Online Impact Wrench Shop And How To Utilize What Is Online Impact Wrench Shop And How To Use schlagschrauber-bewertungen
8 Tips To Improve Your Patio Door Glass Repair Game Patio door Threshold Repair
20 Things You Should Ask About Three Sleeper Bunk Bed Prior To Purchasing Three Sleeper Bunk Bed Bunk Beds Triple (output.jsbin.Com)
Three Greatest Moments In MItolyn History mitolyn Sale
What's The Current Job Market For Replacement Car Keys Kia Professionals Like? Replacement Car Keys Kia
Five Killer Quora Answers On Accident Injury Legal Representation Accident Injury Legal Representation (morphomics.science)
Why You Should Not Think About Improving Your Warming Plate warmhaltecontainer (brewwiki.win)
The 10 Scariest Things About Adult 3 Wheel Scooter Adult 3 Wheel Scooter (Googlino.Com)
5 Myths About Cisco 730 On-Ear Bluetooth Headset That You Should Stay Clear Of Heimkino Leinwand motorisiert
How Door Bottom Seals Has Transformed My Life The Better Weather Seals
See What Coffee Machines Tassimo Tricks The Celebs Are Making Use Of Coffee Machines Tassimo
The 10 Scariest Things About Glass Condensation Repair glass condensation Repair (http://support.roombird.ru)
The 9 Things Your Parents Taught You About Emergency Window Hinge Repairs Emergency Window Hinge Repairs
Fitted Ovens Tools To Ease Your Daily Life Fitted Ovens Trick That Every Person Should Be Able To Fitted oven
Wooden Bunk Beds With Slide Tools To Ease Your Everyday Lifethe Only Wooden Bunk Beds With Slide Trick That Every Person Must Know Wooden Bunk Beds With Slide
Vauxhall Zafira Car Key Replacement Tips To Relax Your Daily Life Vauxhall Zafira Car Key Replacement Trick Every Individual Should Know Vauxhall Zafira Car Key Replacement
Why Everyone Is Talking About Polish Category C Driving License What Can You Drive Today Kupno Prawa Jazdy - historydb.date -
The 10 Scariest Things About Buy UK Driver's License Online Buy UK Driver's License Online - https://canvas.instructure.Com/,
10 Top Mobile Apps For Psychiatrist Appointment private psychiatrist assessment Near me
Buy Tumble Dryers Tips From The Top In The Business kompakte wäSchetrockner (http://Animationfixation.net)
15 Reasons To Not Ignore Hyundai Replacement Car Keys Replacement Hyundai Key
What's The Job Market For Mazda Spare Key Cost Professionals? Mazda Spare Key
Why You Must Experience Dewalt Tool At Least Once In Your Lifetime Dewalt hand tools
10 Things That Your Family Teach You About Tools Dewalt Tools Dewalt [https://graph.org/10-Things-Your-Competitors-Help-You-Learn-About-Dewalt-Tool-Set-10-24]
Five Killer Quora Answers On Upvc Door Panel Renovation UPVC Door Panel Renovation (hedgedoc.digillab.uni-augsburg.de)
You'll Never Guess This Bunk Bed Cheap's Secrets bunk bed cheap
Five Killer Quora Answers To Electric In Wall Fireplace Electric In Wall Fireplace
See What Bedside Cot Beds Tricks The Celebs Are Using Bedside Cot Beds
10 Best Facebook Pages Of All Time Concerning 3 Wheel Stroller Lightweight 3 wheel strollers
You'll Never Be Able To Figure Out This Trusted House Locksmith's Secrets trusted House Locksmith
Can L Shaped Sectional Ever Rule The World? L Shaped Sectionals
An In-Depth Look Into The Future What's In The Pipeline? Structured Driving Lessons Grimsby Industry Look Like In 10 Years? Driving School In Grimsby (clinfowiki.win)
Deep Chest Freezer Tools To Improve Your Everyday Lifethe Only Deep Chest Freezer Trick That Everyone Should Learn Deep Chest Freezer
The No. Question Everybody Working In Apply For A2 Driving License Online Should Be Able Answer führerschein A2 preis
10 Things That Your Family Taught You About Add Online Test Add Online Test
Ten In Built Ovens That Really Change Your Life in Built ovens
10 Sites To Help To Become A Proficient In Bedside Cot For Healthy Sleeping Cotbed With Drawers
9 Lessons Your Parents Teach You About Fridges Online Fridges Online
You'll Never Guess This Renault Key Card Programming Near Me's Secrets Renault Key Card Programming Near Me
It's A Toyota Aygo Key Success Story You'll Never Imagine Toyota Aygo Key Fob
5 Killer Quora Answers On Hire Hacker Online Hire Hacker Online
Three Greatest Moments In Pushchair For Twins History Twin Pushchairs
What's The Job Market For Misted Double Glazing Professionals? Misted Double Glazing
Searching For Inspiration? Look Up House Lock Fix house lock issues
The People Closest To Cordless Tool Set On Account Share Some Big Secrets Akku maschinen set 18v
Guide To Clio Key Replacement: The Intermediate Guide To Clio Key Replacement Clio Key Replacement
Test: How Much Do You Know About Pram For A Newborn? Pushchairs prams
See What American Fridge Freezer Tricks The Celebs Are Utilizing American Fridge Freezer
One Key Trick Everybody Should Know The One Cheap Petrol Chainsaw Trick Every Person Should Be Able To Kärcher HD 5/15 C Plus
What's The Current Job Market For Double Glazing Leak Repair Professionals? Double Glazing Leak Repair
Five Killer Quora Answers To Echo CS-2511TES Chainsaw echo Cs-2511tes chainsaw
The Comprehensive Guide To U Shaped Sofa Large Sectional With Chaise
You'll Never Be Able To Figure Out This Three Wheeled Mobility Scooter's Tricks Three Wheeled Mobility Scooter (www.divephotoguide.Com)
What's The Current Job Market For Best Bean To Cup Filter Coffee Machine Professionals Like? best bean to cup filter coffee machine [bestbeancoffeemachine76285.blogpostie.com]
15 Best Documentaries On I Will Buy A Polish Driving License Prawi Jazdy C
Why Nobody Cares About Electric Impact Wrench GüNstiger Schlagschrauber
Window Frame Repair Tools To Help You Manage Your Daily Lifethe One Window Frame Repair Trick That Every Person Must Be Able To Window Frame Repair (Diego-Maradona.Com.Az)
You'll Never Be Able To Figure Out This Buy Quality Counterfeit Money's Tricks Buy Quality Counterfeit Money
Cots And Cot Beds: The Good, The Bad, And The Ugly cheap baby Cots For sale
Get To Know The Steve Jobs Of The Siemens Home Connect Oven Industry Waschmaschine Aquastop Funktion
See What Kia Picanto Replacement Key Tricks The Celebs Are Making Use Of Kia Picanto Replacement Key
The 10 Most Terrifying Things About Hire Hacker For Icloud hire Hacker for icloud
See What French Door Replacement Tricks The Celebs Are Using French Door Replacement
See What French Refrigerator Tricks The Celebs Are Using French Refrigerator
You'll Never Guess This Window Hinge Replacement's Tricks Window Hinge Replacement - http://wx.abcvote.cn/home.php?Mod=space&uid=5743632,
What's The Job Market For MItolyn Reviews Professionals? mitolyn reviews (https://wodirectory.com/listings13448271/a-look-in-affordable-mitolyn-supplement-s-secrets-of-affordable-mitolyn-supplement)
Ten L Shaped Sofas That Really Change Your Life L Shaped Sofas
This Is The Ugly Truth About Buy Good Headphones Online Headphones Shop
The 10 Most Terrifying Things About Espresso Pod Machine Espresso Pod Machine
Dolce Gusto Pod Machine Tools To Help You Manage Your Everyday Lifethe Only Dolce Gusto Pod Machine Trick That Should Be Used By Everyone Learn Dolce Gusto Pod Machine
How To Know If You're Ready To Go After Freezer Chest Fridge freezer Chest
UPVC Front Door Repair Tools To Help You Manage Your Daily Life UPVC Front Door Repair Trick That Every Person Must Know UPVC Front Door Repair
9 Lessons Your Parents Teach You About Emergency Board Up Company emergency board up Company (http://Bbs.abcdv.net)
You'll Never Guess This Private Psychiatrist UK's Tricks Private Psychiatrist uk
7 Things You've Never Learned About Cheap Loveseats UK best sleeper couch (oh-Noble-3.federatedjournals.com)
You'll Never Be Able To Figure Out This Casement Window Handle Replacement's Benefits Casement Window Handle Replacement
What's The Current Job Market For Self Vacuum Professionals Like? self Vacuum (https://www.udrpsearch.com)
9 . What Your Parents Taught You About Nespresso Espresso Nespresso Espresso
5 Killer Quora Answers On Anti-aging Cellular Repair anti-aging Cellular Repair
Guide To Double Pane Window Repair: The Intermediate Guide Towards Double Pane Window Repair double pane window repair
9 . What Your Parents Teach You About Co Codamol Online Ordering Co Codamol Online Ordering
Five Killer Quora Answers On Compact Cot Travel Cots With Bassinet
How Patio Door Repair Service Near Me Was The Most Talked About Trend Of 2024 Patio Door Panel Repair
See What Circular Saw 18v Tricks The Celebs Are Using Circular Saw 18v
9 Things Your Parents Taught You About Upvc Door Maintenance UPVC Door Maintenance
The 3 Greatest Moments In Compact Washing Machines History top-waschmaschinen
10 Websites To Help You Learn To Be An Expert In Buy Fake Czech Driving License Získejte ČEský Řidičský Průkaz (doc.adminforge.de)
15 Things You Didn't Know About Commercial Pressure Washers Hochdruckreiniger Für Den Hausgebrauch
15 Astonishing Facts About U-Shaped Sectional Large Sectional With Chaise
Where Will Cost Of Window Handle Replacement Be 1 Year From Today? Broken Window Handle
How To Explain Bedside Cot For Modern Nursery To Your Grandparents Cotbed With Drawer
The 10 Most Terrifying Things About Planing Machines For Sale Planing Machines for sale
7 Secrets About Cheap 50L Compressor That Nobody Can Tell You Akku Schlagschrauber 1/2 Zoll Angebot
See What Emergency Glass Repair Tricks The Celebs Are Making Use Of Emergency Glass Repair
Folding Treadmill UK: The Good And Bad About Folding Treadmill UK Portable Treadmill UK
The 9 Things Your Parents Taught You About Tilt And Turn Window Parts Tilt And Turn Window Parts
Twenty Myths About Buy A Cheap Freestanding Hob: Busted Induktionskochfeld Kaufen
Five Killer Quora Answers On Fold Up Electric Wheelchairs Fold Up Electric Wheelchairs
Guide To Three Wheeler Prams: The Intermediate Guide The Steps To Three Wheeler Prams Three Wheeler Prams (http://honghu.cn/home.php?mod=space&uid=1138)
You'll Never Be Able To Figure Out This Mistubishi Asx Car Key's Secrets Mistubishi Asx Car key
5 Killer Quora Answers On Citroen Car Keys citroen Car key
10 Myths Your Boss Has Concerning Volkswagen Key Lost Volkswagen Key
30 Inspirational Quotes About Compact Washing Machines Waschmaschinen-GeschäFt
20 Resources That Will Make You More Successful At Key Fob Porsche Porsche Key Fob
10 Things Your Competition Can Inform You About Convertible Baby Crib Convertible Baby Cribs (kanban.xsitepool.Tu-freiberg.de)
UPVC Door Adjustment Tools To Improve Your Everyday Lifethe Only UPVC Door Adjustment Trick That Everybody Should Know UPVC Door Adjustment
5 Killer Quora Answers To Buy An Oven Set With Hob Buy an Oven Set with Hob
The Reason Window Repair Is Fastly Changing Into The Hottest Trend Of 2024 Window Caulking
You'll Be Unable To Guess Mitolyn Scam Or Legit's Tricks Mitolyn Scam Or Legit
The 9 Things Your Parents Taught You About House Lock Maintenance house lock maintenance
Where Do You Think Patio Door Repair Company Be One Year From Right Now? Patio Door Glass Replacement
Where Do You Think Adult Metal Bunk Beds One Year From This Year? Triple Adult Bunk Beds (hikvisiondb.webcam)
9 Lessons Your Parents Taught You About Coffee Bean Coffee Machine coffee bean coffee Machine
10 Key Factors Concerning Secure Austrian Drivers License You Didn't Learn In School echter ÖSterreichischer führerschein zu verkaufen
20 Things That Only The Most Devoted Buy Washer And Dryer Together Fans Should Know top-marken für Waschtrockner
Why We Our Love For Replacement Key For Volvo V50 (And You Should Also!) Replacement Key For Volvo V50 Near Me
What's The Current Job Market For Volvo Spare Key Professionals Like? volvo spare key
5 Hand Drill Lessons From The Pros Akkubohrmaschine Test (hack.allmende.io)
A An Overview Of Bunk Bed Adult From Start To Finish Adult Bunk
Question: How Much Do You Know About French Driving License Online? renouvellement Du permis de conduire Français
The 10 Most Scariest Things About Subaru Outback Key Fob Subaru Outback Key Fob
Learn What ADHD Assessments Cardiff Tricks The Celebs Are Using private adhd assessment online (md.Ctdo.de)
10 Things That Your Family Teach You About Small Window Handle Replacement Small Window Handle Replacement - 80aaaokoti9eh.рф,
8 Tips To Increase Your Best Cots Game which travel cot
Guide To Tilt And Turn Window Locking Mechanism Repair: The Intermediate Guide In Tilt And Turn Window Locking Mechanism Repair tilt and Turn Window locking mechanism repair
You'll Never Guess This Robot Vacuum With Self Emptying's Secrets Robot Vacuum With Self Emptying
The 10 Scariest Things About L Shaped Sofa Couch l shaped sofa couch
3 Ways That The TestDaF Certificate Can Affect Your Life test daf zertifikat; https://md.swk-web.Com/agm10ya2r3kysv7dib89ma,
You'll Be Unable To Guess Sash Window Installers Nearby's Tricks Sash window Installers nearby, autocela.lv,
The Best U Shaped Sectional Tricks To Transform Your Life best u shaped sectional
The 9 Things Your Parents Taught You About Old Window Handle Replacement Old Window Handle Replacement
15 Funny People Working Secretly In ADHD Assessment UK Private private adhd diagnosis london (https://www.pathofthesage.com/members/sisterrake50/activity/673479/)
It's The Complete List Of Belgian Driving License For Sale Dos And Don'ts Belgisch Rijbewijs (Postheaven.Net)
14 Smart Ways To Spend Your Extra Money L-Shaped Couch Budget Best L-Shaped Couches
The Guide To ADHD Assessment For Adults Private In 2024 adhd Assessment cost
Are You Getting The Most Value From Your Siemens Home Connect Oven? siemens Waschmaschine Erfahrungen
5 Bridgestone Turanza 6 Price Comparison Lessons From Professionals Hankook Ventus Prime 4 Test
See What MDMA Pills Online Tricks The Celebs Are Utilizing mdma pills online
9 Things Your Parents Taught You About Driving Schools Grimsby Driving Schools Grimsby
9 . What Your Parents Taught You About Hand Mitre Saw Hand Mitre Saw (elearnportal.science)
Five Killer Quora Answers To Treadmill For Home With Incline treadmill for home with incline
Why We Love Bedside Cot For Contemporary Design (And You Should Also!) Cot Bed With Storage (Platform.joinus4health.eu)
The Top Guttering Repairs Tricks For Changing Your Life Top Guttering
Five Reasons To Join An Online Freezer With Delivery And Connection Shop And 5 Reasons You Shouldn't Gefrierschrank Mit Schubladen Günstig
B1 German Certificate Tips To Relax Your Daily Life B1 German Certificate Trick That Everybody Should Know B1 German Certificate
Integrated Cooker And Hob Tools To Ease Your Everyday Lifethe Only Integrated Cooker And Hob Trick That Everyone Should Know integrated Cooker and hob
See What Window Seal Repair Tricks The Celebs Are Making Use Of Window Seal Repair
10 Things Everybody Hates About Bedside Cot For Newborn Baby Bedside Crib For Small Spaces
The Top Weight Loss Medications Experts Are Doing 3 Things Order Weight Loss Medications
A Peek Inside The Secrets Of Portable Bedside Crib wooden cot bed with drawer
What's The Job Market For Intergrated Kitchen Professionals Like? Intergrated kitchen
7 Simple Tricks To Totally Rocking Your UPVC Door Fix upvc Door fixing
From All Over The Web The 20 Most Amazing Infographics About Chisel Hammer With Hex Shank abbruchhammer mit sds-max aufnahme und vibrationsdäMpfung test
9 Signs That You're A L-Shape Couch Expert L-Shaped Couch
10 Healthy 3 Wheeler Off Road Buggy Habits 3 Wheeler buggies - lillelund-frederiksen.federatedjournals.com -
Inverter Welding Machine 200a Review Tools To Ease Your Daily Life Inverter Welding Machine 200a Review Trick That Every Person Must Be Able To Inverter Welding Machine 200A Review
Don't Buy Into These "Trends" Concerning Compressor With Air Tools Buy Top-Kompressor Online Kaufen (case.Edu)
What's The Current Job Market For Contemporary Electric Fireplace With Mantel Professionals? Contemporary Electric Fireplace With Mantel
The Most Hilarious Complaints We've Been Hearing About Industrial Planing Machines Hobelmaschinen-Typen
10 Tips To Know About Ovens On Sales Hobs Oven
5 Killer Quora Answers To Mini Key Replacement mini Key replacement
10 Quick Tips About Replacement Mercedes Key Cost Replacement Mercedes Keys
How Reclining U-Shaped Sectional Was The Most Talked About Trend In 2024 Sofa With Chase
UPVC Door Realignment Tools To Make Your Everyday Lifethe Only UPVC Door Realignment Technique Every Person Needs To Know UPVC Door Realignment
The 10 Scariest Things About Order Professional Tools Online Order Professional Tools Online
The Best Digital Signage Display Strategies For Changing Your Life Bang & Olufsen Beoplay H95 Angebot [https://gettydirectory.com/]
Land Rover Car Key Replacement: 11 Thing That You're Failing To Do Replacement Land Rover Key
You'll Never Be Able To Figure Out This Double Glazing Fog's Tricks double glazing fog
Guide To UPVC Door Mechanism Repair: The Intermediate Guide On UPVC Door Mechanism Repair UPVC Door Mechanism Repair (Uvs2.net)
ADHD Psychiatrist Tips To Relax Your Everyday Lifethe Only ADHD Psychiatrist Trick Every Individual Should Learn ADHD Psychiatrist
Motorized 3 Wheel Scooter Techniques To Simplify Your Everyday Lifethe Only Motorized 3 Wheel Scooter Trick That Every Person Should Learn Motorized 3 Wheel Scooter
See What Dewalt Battery Tools Tricks The Celebs Are Using dewalt battery Tools
The Best Robot Vacuums And Mops Tricks To Rewrite Your Life Best Robot Vacuums
See What Seal Failure In Windows Tricks The Celebs Are Using Seal Failure In Windows
See What Quiet Wine Cooler Tricks The Celebs Are Using Quiet Wine Cooler
A Trip Back In Time: What People Discussed About French Door Refrigerator 20 Years Ago French Door Refrigerator Sale (Telegra.Ph)
This Week's Most Remarkable Stories About Mobility Scooter Near Me Mobility Equipment
The Secret Secrets Of Private Adult ADHD Assessment Near Me private practice psychiatrist near me
The Worst Advice We've Ever Heard About Dolce Gusto Coffee nescafe dolce gusto Coffee maker
9 . What Your Parents Teach You About Key Seat key seat (https://mozillabd.science/wiki/20_Trailblazers_leading_the_way_in_seat_cordoba_key_replacement)
Why Affordable French Driving License Still Matters In 2024 obtenir le permis de conduire françAis
Guide To Coffee Beans UK 1kg: The Intermediate Guide In Coffee Beans UK 1kg Coffee Beans UK 1Kg
You'll Never Be Able To Figure Out This Mitolyn Scam Or Legit's Tricks mitolyn scam or legit (122.116.190.233)
Nine Things That Your Parent Teach You About Wholesale Coffee Beans Wholesale Coffee Beans (canvas.instructure.com)
What's The Current Job Market For Vinyl Gasket Replacement Professionals Like? vinyl Gasket replacement (https://Test.annelertoplandik.com/User/lizardcolt32)
20 Bedside Cot For Convertible Use Websites Taking The Internet By Storm Cot Bed With Storage Drawer
Guide To Best Urolithin A Supplement: The Intermediate Guide Towards Best Urolithin A Supplement Best Urolithin A supplement
The Secret Secrets Of Counterfeit Money Expert On The Darknet falschgeld Darknet marktplatz
Why You Should Focus On Improving Bunk Bed For 3 Triple Bunk Bed 3 Single Beds
The 10 Scariest Things About Electric Bariatric Wheelchair Electric Bariatric Wheelchair
Guide To Temporary Boarding: The Intermediate Guide The Steps To Temporary Boarding Temporary Boarding
Five Killer Quora Answers On ADHD Online Test ADHD Online Test
Angle Grinder With Speed Control 125mm In A Case Offer: Myths And Facts Behind Angle Grinder With Speed Control 125mm In A Case Offer akku schlagschrauber auf rechnung
Guide To Smart Vacuum Self Emptying: The Intermediate Guide On Smart Vacuum Self Emptying Smart Vacuum Self Emptying [ai-db.science]
Five Killer Quora Answers On Mitolyn Supplements Mitolyn supplements
Wine Fridge Uk Tools To Ease Your Daily Lifethe One Wine Fridge Uk Trick That Everyone Should Be Able To Wine fridge uk
15 Top House Locksmith Services Bloggers You Need To Follow Top House Locksmith
The Best Advice You'll Ever Receive About Window Handle Replacement Andersen Window Handle Replacement
Ten Robot Vacuum Mops That Really Improve Your Life Robot Vacuum Mops
9 Lessons Your Parents Teach You About Sash Window Replacement Specialists Sash Window Replacement Specialists
See What Child Cot Bed Tricks The Celebs Are Using Child Cot Bed
The Best Robotic Vacuum Cleaner UK Tricks For Changing Your Life best robotic Vacuum cleaner uk
You'll Never Guess This Sash Window Refurbishing Company's Secrets Sash Window Refurbishing Company
15 Gifts For The Bedside Cot For Safe Infant Sleep Lover In Your Life cot with storage Drawer (discoveringalifeyoulove.com)
You'll Never Guess This Key Ignition Repair's Tricks Ignition Repair
15 Shocking Facts About Buy Washer Online You've Never Known Waschmaschinen-Lieferung
You'll Never Guess This Porsche Key Programmer's Benefits Porsche Key Programmer
Everything You Need To Be Aware Of Drill Comparison bohrmaschine online bestellen
The Most Pervasive Issues In Warming Plate Thekenvitrine
Car Key Replacement Mitsubishi Tools To Make Your Daily Lifethe One Car Key Replacement Mitsubishi Trick That Every Person Should Be Able To Car Key Replacement Mitsubishi (https://md.Swk-web.com)
What's The Job Market For Top Double Glazing Companies Professionals? Double Glazing companies
How To Tell If You're Ready For Electric Drill Schlagbohrmaschine GüNstig (Securityholes.Science)
What's The Job Market For Full Mental Health Assessment Online Professionals? Full Mental Health Assessment Online
The 10 Scariest Things About Vw Car Key Replacement Cost Vw Car Key
Five Killer Quora Answers To Dewalt Garden Tools dewalt garden tools (https://fancypad.techinc.nl/hqvdmhqls3qqfjtbqbxkmq/)
5 Laws That Will Help The Belgium Driving Permit For Sale Industry Bestel Een Belgisch Rijbewijs
10 Ways To Create Your Honda Key Empire Honda key fobs (45.55.138.82)
The 10 Scariest Things About Bariatric Self Propelled Wheelchairs Bariatric Self Propelled Wheelchairs
Which Built In Oven To Buy Tools To Streamline Your Daily Lifethe One Which Built In Oven To Buy Trick Every Individual Should Know which built In oven to buy
What's The Job Market For Vauxhall Car Key Replacement Near Me Professionals? vauxhall car key replacement near me (notes.io)
The Reason Everyone Is Talking About Fluid-Cored Wire Welding Machine Without Gas Reviews This Moment metallbandsäge schwenkbar
14 Savvy Ways To Spend Extra Goethe A1 Certificate Budget goethe-zertifikat Kaufen
How Robotic Vacuum Was The Most Talked About Trend Of 2024 Vacuum robot (pad.stuve.de)
The 10 Scariest Things About Triple Bunk Beds For Adults Triple Bunk Beds For Adults
9 Lessons Your Parents Taught You About Seat Ibiza Car Key Replacement seat ibiza Car key replacement
What's The Job Market For Nissan Juke Replacement Key Professionals? Nissan Juke Replacement Key
Five Killer Quora Answers On Skoda Citigo Key Replacement Skoda Citigo Key Replacement
It's Enough! 15 Things About Window Hinge Repair Specialist We're Overheard Repair Window Hinges
The 10 Scariest Things About Specialty Window Handle Replacement Specialty Window Handle Replacement
Mitsubishi Lancer Remote Start's History History Of Mitsubishi Lancer Remote Start replacement car Key mitsubishi
See What Restore UPVC Doors Tricks The Celebs Are Using Restore UPVC Doors
9 Things Your Parents Teach You About Window Hinge Replacement Specialist Window Hinge Replacement Specialist
14 Businesses Doing A Superb Job At Belgium Driving Permit For Sale koop een legaal belgisch rijbewijs
Guide To Tilt And Turn Window Locking System Repair: The Intermediate Guide In Tilt And Turn Window Locking System Repair tilt and turn window locking system repair - md.ctdo.De -
U Sectional Couch Tools To Ease Your Daily Life U Sectional Couch Trick That Everybody Should Know U Sectional Couch (md.chaosdorf.de)
A Productive Rant About Order A2 Motorcycle License Online FüHrerschein Klasse A2 GüNstig
Are You In Search Of Inspiration? Look Up Buy A Drivers License In Poland Kup Prawo Jazdy W Polska
9 . What Your Parents Teach You About Bunk Bed For Teens Bunk bed for Teens
You'll Never Guess This Free Online ADD Test's Tricks Free Online ADD Test (liverstitch10.bravejournal.net)
What's The Current Job Market For Double Pram Professionals Like? Double Pram
The Most Hilarious Complaints We've Been Hearing About Electric Integrated Oven integrated oven and hob electric
The 10 Most Scariest Things About Tilt And Turn Window Restoration Tilt And Turn Window Restoration
The 10 Most Scariest Things About Tilt And Turn Window Renovation Tilt And Turn Window Renovation (pad.stuve.de)
20 Trailblazers Lead The Way In Mental Health Assessment Comprehensive Mental Health Assessment [md.chaosdorf.de]
The 9 Things Your Parents Taught You About Crib That Turns Into Bed Crib That Turns Into Bed
Why We Enjoy Peugeot Car Key (And You Should Too!) Peugeot Key
Stylish Rollator Walker Tools To Make Your Everyday Lifethe Only Stylish Rollator Walker Technique Every Person Needs To Know Stylish Rollator Walker
See What Double Pushchair Tricks The Celebs Are Making Use Of Double Pushchairs
Buy Fridge UK: The Good, The Bad, And The Ugly waschmaschine 9kg angebot
"The Ultimate Cheat Sheet For Cordless Power Tool Sets Cordless Tool Sets
5 Killer Quora Answers On Refrigerator With Wine Rack Refrigerator With wine rack
The 9 Things Your Parents Taught You About Durable Window Handle Replacement durable window handle replacement
See What Pullout Couch Tricks The Celebs Are Making Use Of Pullout Couch
5 Killer Quora Answers To Husqvarna 572 XP Chainsaw Review Husqvarna 572 XP Chainsaw Review
The 10 Scariest Things About Modern Handmade Sectional Handmade Sectional
Its History Of Integrated Oven integrated electric oven (swaay.com)
17 Reasons Not To Ignore Top-Rated Compressor Online Kleiner Luftkompressor Kaufen
You'll Never Guess This Affordable Window Repair's Secrets emergency window repair
You'll Never Guess This 24-Hour House Locksmith's Tricks 24-Hour House Locksmith
20 AEG Built-In Oven Deal Websites Taking The Internet By Storm waschmaschine 7 kg angebot (theflatearth.win)
What's The Current Job Market For Nissan Juke Replacement Key Professionals Like? Nissan Juke Replacement Key (https://harper-lykke.blogbright.net/five-lessons-you-can-learn-from-nissan-key-replacement)
You'll Never Guess This Refrigerator French Doors's Benefits refrigerator French door
10 Best Ovens That Are Unexpected Buy a oven
Five Killer Quora Answers On How Much Is An ADHD Assessment How Much Is An ADHD Assessment (oakmontforum.Com)
See What Peugeot Partner Key Fob Tricks The Celebs Are Using Peugeot Partner Key Fob
A An Overview Of Coffee Makers Online From Start To Finish buy coffee makers online
Guide To U Shaped Corner Sofa: The Intermediate Guide For U Shaped Corner Sofa U Shaped Corner Sofa
Why Hungarian Driver's License Validity Could Be Your Next Big Obsession? Jogos Vezetői Engedély Vásárlása
You'll Never Guess This Patio Door Frame Repair's Tricks Patio Door Frame Repair
Ten Buy Cheap Steroids Germanys That Really Improve Your Life Seriöse Steroid-Websites Deutschland (hedge.fachschaft.informatik.Uni-kl.de)
13 Things You Should Know About Cheap ADHD Assessment That You Might Not Have Known Cost Of ADHD Assessment
5 Laws That Will Help In The Complete Tire Deals Industry Neue Sommerreifen Kaufen - sciencewiki.science,
The Reasons Why Drinks Machine Tassimo Is The Obsession Of Everyone In 2024 Tassimo Drinks Machine
See What Mitolyn Supplement Official Website Tricks The Celebs Are Utilizing Mitolyn Supplement Official Website
See What Ford Car Key Replacement Tricks The Celebs Are Utilizing Ford car key Replacement
10 Things People Hate About Nissan Key Replacement Near Me Nissan Keys Replacements
The Biggest Issue With ADHD Test Free And How You Can Fix It Adult ADHD Test Online
Guide To Fridge For Wine: The Intermediate Guide The Steps To Fridge For Wine Fridge For Wine
Guide To Bedside Cot For Baby's Room: The Intermediate Guide For Bedside Cot For Baby's Room Bedside Cot For Baby's Room (hack.allmende.io)
15 Planing Machines Brands Benefits Everybody Must Be Able To Hobelmaschinen in meiner Nähe (writeablog.net)
Are You Tired Of Window Hinge Fix? 10 Inspirational Resources To Rekindle Your Love Window Hinge Maintenance
How To Save Money On Cordless Machine Akku-Werkstattwerkzeuge Kaufen
What's The Current Job Market For Slide For Bunk Bed Professionals? Slide For Bunk Bed (www.guzhen0552.cn)
7 Simple Strategies To Completely Refreshing Your Cheap Tumble Dryers Online WäSchetrockner Kaufen
Nine Things That Your Parent Taught You About Container 6 Feet Container 6 feet
You'll Be Unable To Guess Barista Espresso Machine's Secrets barista espresso Machine (brewwiki.win)
Five Killer Quora Answers To Mitre Saw Offers Mitre Saw Offers
What Is Wine And Beer Fridge And Why Is Everyone Speakin' About It? fridge for wine
10 Tell-Tale Signs You Must See To Know Before You Buy Ultra Modern Sofas UK sofa Couch uk
The 12 Worst Types Of Users You Follow On Twitter goethe c1 zertifikat
You'll Be Unable To Guess Bunk Bed With Slide Uk's Benefits Bunk Bed With Slide Uk
15 Pinterest Boards That Are The Best Of All Time About Window Pane Repair Misted Window Pane Repair - test.annelertoplandik.com -
The Top Reasons People Succeed On The Electric Height-Adjustable Desk Industry Escritorios Eléctricos De Altura Ajustable
5 Killer Quora Answers On Sash Window Replacement Cost sash Window replacement cost
The Hidden Secrets Of Replacement Vauxhall Car Key how much for a replacement vauxhall car key (https://hensley-dall.thoughtlanes.net/the-top-vauxhall-mokka-replacement-key-gurus-do-3-things)
5 Killer Quora Answers On Mercedes Replacement Key Cost UK Mercedes Replacement Key Cost
10 Life Lessons We Can Learn From Private Psychiatrists psychiatrists Private; pad.Stuve.de,
Door Handle Replacement Tips That Will Transform Your Life door Handle Mechanic
Volvo Replacement Key Techniques To Simplify Your Daily Lifethe One Volvo Replacement Key Trick That Should Be Used By Everyone Be Able To Volvo Replacement Key - Https://rehabsteve.com -
Nine Things That Your Parent Taught You About 3 Wheeler Travel System 3 Wheeler Travel System
Speak "Yes" To These 5 Drinks Machine Tassimo Tips Tassimo Drinks Machine
The Three Greatest Moments In Gutters History Roof Drainage
You'll Never Guess This Professional Electric Treadmills's Secrets Professional Electric Treadmills
11 Strategies To Completely Redesign Your Tassimo Coffee Machine bosch Tassimo machine
10 Websites To Help You Learn To Be An Expert In Window Pane Repair Glass repair
14 Smart Ways To Spend Your The Leftover Wood Cot Budget Natural Wood Cots
What's The Current Job Market For Tasimo Coffee Machines Professionals Like? Tasimo Coffee Machine
The 10 Scariest Things About Tilt And Turn Window Professionals Tilt And Turn Window Professionals (https://41-4lcpj.укр/user/toweractor24)
Learn About Best Angle Grinder While Working From At Home Best Angle Grinders
10 Fundamentals To Know Small Cots You Didn't Learn At School Travel Cot With Bassinet
You'll Never Guess This Cheap Counterfeit Money's Tricks Cheap Counterfeit Money
Nine Things That Your Parent Taught You About Commercial Window Repair commercial window Repair
5 512GB Gaming Smartphone Lessons Learned From The Professionals Videowand Halterung
Why You Should Focus On Improving Patio Doors Repairs Sliding Glass Patio Door Repairs
Five Killer Quora Answers To Baby Bed Cot Baby Bed Cot (urlscan.io)
What's The Current Job Market For Premium Handmade Sofa Designs Professionals Like? Premium Handmade Sofa Designs
What's The Job Market For UPVC Door Company Professionals Like? UPVC Door Company
14 Businesses Doing A Superb Job At Impact Wrench Store Kfz-Schlagschrauber (md.swk-web.com)
Nine Things That Your Parent Taught You About Robot Mop UK robot mop uk
15 Of The Most Popular Pinterest Boards Of All Time About Planing Machines For Carpentry Hobelmaschinen-Typen
The 10 Scariest Things About Freezer With Delivery And Connection Freezer With Delivery And Connection
What Is Bedside Crib With Wheels And Why Is Everyone Talking About It? Cot Drawer
Guide To All Terrain Travel System: The Intermediate Guide For All Terrain Travel System All Terrain Travel System
10 Strategies To Build Your Best Milling Machines Empire fräsmaschinen mit ratenzahlung kaufen
5 Laws That Will Help The Norwegian Driving License Supplier Industry pris på norsk førerkort
What's The Job Market For How To Get A Nissan Key Made Professionals Like? How To Get A Nissan Key Made
The 10 Scariest Things About Authentic Irish Driver's License authentic irish driver's license
15 Funny People Working In Couch For Sale Near Me In Couch For Sale Near Me cheap Couches Uk
10 Healthy Pull Out Bed Habits Sectional With Pullout Bed
20 Myths About Asus Zenfone 12 Ultra: Busted philips 75pus7009/12 smart tv (https://Welter-vertrieb72968.blogspothub.com/37696429/the-10-worst-120-inch-fixed-frame-screen-fails-of-all-time-could-have-been-prevented)
Five Killer Quora Answers To Plasma Cutter Test 2024 Mig Mag SchweißGeräT Set Angebot
See What Door Panel Specialists Tricks The Celebs Are Using Door Panel Specialists
What's The Current Job Market For Private ADHD Assessment Adults Professionals Like? private adhd assessment Adults
You'll Never Guess This Range Rover Keys's Tricks Range Rover Keys (hedge.fachschaft.informatik.uni-kl.de)
How Can A Weekly Toyota Replacement Key Project Can Change Your Life Replacement Toyota Key
"Ask Me Anything," 10 Answers To Your Questions About Lexus Key Fob Lexus Key Fob Replacement Cost
Your Worst Nightmare Concerning Affordable Planing Machines It's Coming To Life Hobelmaschinen Für Die Zimmerei
Guide To Mobility Scooters Shops Near Me: The Intermediate Guide On Mobility Scooters Shops Near Me mobility scooters shops near me
Five Killer Quora Answers On Hyundai I10 Key Fob Replacement Hyundai I10 Key Fob Replacement
The 10 Most Terrifying Things About Lexus Replacement Key Lexus Replacement Key
See What Sliding Door Seals Tricks The Celebs Are Making Use Of Sliding Door Seals
The 10 Most Scariest Things About Washing Machine Bundles Waschmaschinen-Rabatte
20 Fun Informational Facts About Washer Dryer Combo With Warranty sonderangebote FüR Waschtrockner-kombinationen
Guide To Land Rover Discovery 3 Replacement Key: The Intermediate Guide In Land Rover Discovery 3 Replacement Key Land Rover Discovery 3 Replacement Key - suncheng.asia -
Dewalt Electric Hand Tools Tips To Relax Your Daily Lifethe One Dewalt Electric Hand Tools Trick That Every Person Must Be Able To Dewalt Electric Hand Tools; https://Articlescad.com/10-reasons-That-people-are-hateful-of-dewalt-power-tool-sets-365532.html,
10 Things People Hate About Crib That Turns Into Toddler Bed Convertible Cribs
This Is The Advanced Guide To Fear Of Driving Lessons führerschein Kaufen darknet
Why Is Power Tool Combo So Famous? Power Tool Combo Set (Googlino.com)
What Is Psychiatric Assessment Near Me And How To Use It private psychiatry clinic
The Unspoken Secrets Of Frost Free Chest Freezer Chest Fridges
What's The Current Job Market For UPVC Door Panel Replacement Professionals Like? UPVC Door Panel Replacement (http://t.044300.net/home.php?mod=space&uid=2292580)
Why Seat Key Fob Is A Must At The Very Least Once In Your Lifetime seat key fob replacement
9 Things Your Parents Taught You About House Door Lock Service House Door Lock Service
The 10 Most Terrifying Things About 3 Wheel Mobility Solution 3 Wheel Mobility Solution
The 10 Most Scariest Things About Nissan Qashqai Key Replacement Nissan Qashqai Key Replacement
Ten Pinterest Accounts To Follow About Conservatory Roof Restoration Lock Maintenance
The 10 Scariest Things About Wheelchair Foldable Lightweight Wheelchair Foldable Lightweight - marocbikhir.com -
9 . What Your Parents Taught You About Residential Window Repair residential Window Repair
5 Laws That Will Help With The Bedside Cot That Attaches To Bed Industry Cot Drawers (Jszst.Com.Cn)
10 Best Facebook Pages Of All Time About Baby Cot Portable Cot
How To Tell The Good And Bad About Small U Shaped Sofa Sofa W Chaise
15 Twitter Accounts You Should Follow To Learn More About Buy Novelty Belgium Driver's License Europees Rijbewijs Online Kopen
10 Websites To Help You Learn To Be An Expert In Ovens Sales hobs With oven
The 10 Scariest Things About ADHD Test Online For Adults ADHD Test Online For Adults (Https://Hikvisiondb.Webcam/Wiki/DIVA_5_Test_Online_10_Things_Id_Loved_To_Know_Sooner)
Misted Double Glazing Solutions Tools To Improve Your Daily Lifethe One Misted Double Glazing Solutions Trick That Should Be Used By Everyone Know Misted Double Glazing Solutions
What Is Goethe C1 Certificate And Why Are We Talking About It? B1 Zertifikat Kaufen
See What Self Folding Mobility Scooters Tricks The Celebs Are Making Use Of Self Folding Mobility Scooter
Buy Driver's License In Spain Tools To Improve Your Everyday Lifethe Only Buy Driver's License In Spain Trick That Every Person Should Know Buy Driver's License In Spain
What's The Job Market For Mini Cooper Spare Key Professionals Like? Mini Cooper Spare Key
5 Killer Quora Answers On American Style Freezer American Style Freezer
14 Smart Strategies To Spend Extra Top-Rated Milling Machines Budget Kompakte Fräsmaschinen Kaufen
10 Comfortable Sofas UK Tricks All Experts Recommend couch or sofa uk
See What Repair Broken Tilt And Turn Windows Tricks The Celebs Are Utilizing Repair Broken Tilt And Turn Windows (https://fix.mudanauto.com)
The Best Bunk Beds On Sale Tricks To Transform Your Life best bunk bed
UPVC Door Company Tools To Streamline Your Daily Life UPVC Door Company Trick That Every Person Should Know UPVC Door Company
You'll Never Guess This Conservatory Repairs's Tricks Conservatory Repairs (1V34.Com)
Five Killer Quora Answers To Buy Genuine Driving License buy genuine driving license
What's The Current Job Market For Bedside Cot For Stylish Sleep Space Professionals? Bedside Cot For Stylish Sleep Space
Ten Professional Driving License Provider That Will Help You Live Better Hamis Vezetői Engedély Vásárlása
A Guide To Subarucar Key Replacement From Beginning To End Subaru Car Key
The 10 Most Terrifying Things About Misted Window Repair Kit Misted window repair kit
The Lesser-Known Benefits Of Mitolyn Buy mitolyn official Website buy, telegra.ph,
Why You'll Definitely Want To Learn More About Car Key Replacement BMW New BMW Key
Why You Should Focus On Enhancing Chisel Hammer With Hex Shank Akku BandsäGe FüR Metallrohre 18V BüRstenlos Preisvergleich
What Will U Shaped Sectional Be Like In 100 Years? Chaise Lounge Couch
Say "Yes" To These 5 Commercial Grinding Machines Online Tips Elektrische Schleifmaschinen Online Kaufen
What's The Current Job Market For Mazda Lost Keys Professionals Like? Mazda Lost Keys (Http://39.108.172.131/)
How Much Does A B1 Exam Cost 101 Your Ultimate Guide For Beginners B1 Sertifikat
10 Inspiring Images About Best Fridge UnterbaufäHige Waschmaschine Mit 8kg FassungsvermöGen
See What Volkswagen Key Cutting Tricks The Celebs Are Making Use Of Volkswagen Key Cutting
You'll Be Unable To Guess Fiat Tipo Replacement Key's Secrets fiat tipo replacement key (git.Old-craft.Ru)
The Top Companies Not To Be Watch In Order Real Banknotes Industry FäLschungen Kaufen
A Look Into The Future What Is The Portable Electric Treadmills Industry Look Like In 10 Years? Electric Treadmill Comparison
The 10 Scariest Things About Weather Seal Replacement Seal Replacement
Five Killer Quora Answers To Electric Fireplace Wall Mounted Electric Fireplace Wall Mounted
Guide To Cost Of ADHD Assessment UK: The Intermediate Guide For Cost Of ADHD Assessment UK Cost Of ADHD Assessment UK
20 Fun Facts About MItolyn Side Effects affordable mitolyn Supplement
A Trip Back In Time The Conversations People Had About Buy Legal Driver's License 20 Years Ago Schnellverfahren Zum FüHrerschein
See What Saab 93 Replacement Key Tricks The Celebs Are Using Saab 93 Replacement Key
5 Killer Quora Answers On Chest Freezer Large Chest Freezer Large
Five Killer Quora Answers To L Shape Sectional Sofa l shape sectional sofa
7 Tips About 1000 Watt Impact Drill Test Comparison That No One Will Tell You Bohrmaschine Preis
5 Killer Quora Answers To Ketamine Online Fast Shipping Ketamine Online Fast Shipping
10 Websites To Help You To Become An Expert In Misted Windows double glazing condensation
Five Killer Quora Answers To Lightweight Folding Wheelchair UK Lightweight Folding Wheelchair UK
What's The Current Job Market For ADHD Test For Adults Online Professionals Like? ADHD Test For Adults
The 10 Most Terrifying Things About Mazda 2 Car Key Replacement Mazda 2 Car Key Replacement
12 Companies Leading The Way In Mitochondrial Health Supplements Buy Mitolyn Supplement Online
Guide To Strollers 3 Wheels: The Intermediate Guide To Strollers 3 Wheels Strollers 3 Wheels
How To Outsmart Your Boss On De Longhi De'longhi Espresso Machines
How To Resolve Issues With Refrigerator Without Freezer Compartment kühl-gefrier-Kombination kaufen (Git.4lcap.Com)
Five Killer Quora Answers To Tassimo Coffee Machine tassimo coffee machine prices
What's The Job Market For Side Sleeping Crib Professionals? Side Sleeping Crib
9 . What Your Parents Teach You About Free ADHD Online Test ADHD Online Test
See What Outdoor Fireplaces For Sale Tricks The Celebs Are Utilizing Outdoor Fireplaces For Sale (Https://Zenwriting.Net)
You'll Never Be Able To Figure Out This Reclining U-Shaped Sectional's Tricks Reclining U-shaped sectional
Technology Is Making Adult Psychiatry Better Or Worse? Private pay psychiatrist Near me
What's The Current Job Market For Foggy Window Replacement Professionals Like? Foggy Window Replacement
What Is The Heck What Exactly Is Patio Screen Door Repair? Residential Patio Door Repairs
The 10 Scariest Things About Vw Car Key Replacement Cost Vw Car Key Replacement
The 9 Things Your Parents Teach You About Best Cordless Grinder best cordless Grinder (md.un-hack-bar.De)
What's The Current Job Market For Foggy Window Repair Professionals Like? Foggy Window Repair
Wall Mounted Electric Fireplace Tools To Ease Your Everyday Lifethe Only Wall Mounted Electric Fireplace Trick Every Individual Should Learn Wall Mounted Electric Fireplace
Aluminum Door Seals Tools To Make Your Everyday Lifethe Only Aluminum Door Seals Trick That Every Person Must Learn Aluminum Door Seals
What's The Current Job Market For Window Moisture Removal Professionals? Window Moisture Removal
4 Dirty Little Details About Ergonomic Desks Online And The Ergonomic Desks Online Industry estructuras ajustables para escritorios de pie
Double Mitre Saw Tools To Ease Your Daily Life Double Mitre Saw Trick That Should Be Used By Everyone Be Able To Double Mitre Saw
Off Road Prams Tools To Make Your Daily Life Off Road Prams Trick Every Person Should Be Able To Off Road Pram
You'll Never Be Able To Figure Out This Home Treadmill With Incline's Tricks Home Treadmill With Incline
The 10 Most Scariest Things About Suzuki Alto Replacement Key Suzuki Alto Replacement Key
You'll Never Guess This Window Repair Service's Secrets Window Repair Service
See What Cozy Sofa Bed Tricks The Celebs Are Using Cozy Sofa Bed
What's The Job Market For Best Coffee Machine Online Professionals Like? best coffee machine online
20 Fun Facts About Small Cots Travel Cots For Babies
9 Lessons Your Parents Teach You About Sash Window Replacement Specialists Sash Window Replacement Specialists
8 Tips To Increase Your Danish Driver's License Benefits Game Specialist I Dansk Kørekort
10 Things People Hate About Sofa Handmade Leather Sofa
A Brief History Of The Evolution Of Polish Driving License Purchase Polska Agencja Ds. Praw Jazdy (md.Un-hack-bar.de)
15 Best Twitter Accounts To Discover Washing Machine Bundles Neueste Waschmaschinen
Best Integrated Cooker Tools To Streamline Your Daily Life Best Integrated Cooker Trick Every Person Should Know best Integrated cooker
15 Interesting Facts About Sweeper For Sidewalks At A Great Price That You Never Knew kettensäge test
See What 30 Ft Container Price Tricks The Celebs Are Using 30 Ft Container Price
Toyota Prius Key Replacement Cost UK Tools To Help You Manage Your Daily Lifethe One Toyota Prius Key Replacement Cost UK Trick That Everyone Should Know Toyota Prius Key Replacement Cost Uk
How To Make An Amazing Instagram Video About Cordless Nail Guns For Sale akku multifunktionswerkzeug Oszillierend mit zubehör koffer test
How Three Wheel Pushchair Was The Most Talked About Trend In 2024 3 Wheeler Prams
5 Arguments Bosch Built-In Oven Pyrolysis Is Actually A Great Thing Bosch Frontlader Waschmaschine 9 Kg Serie 6 Kaufen
You'll Never Guess This Window Parts Replacement's Tricks Window Parts Replacement
5 Killer Quora Answers On BMW New Key BMW New Key
You'll Never Guess This Quiet Window Handle Replacement's Benefits Quiet Window Handle Replacement
20 Residential Property Locksmith Websites That Are Taking The Internet By Storm house locksmith Company
How To Get More Benefits With Your Triple Bed Bunk Triple Bed Bunk Beds
How Cordless Impact Wrench Influenced My Life For The Better Bester Schlagschrauber
Who Is Responsible For The 10 Kg Capacity Washing Machine Budget? 12 Ways To Spend Your Money siemens Backofen home connect
You'll Never Guess This ADHD Test Online Adults's Tricks Adhd Test Online Adults - Https://Hedge.Fachschaft.Informatik.Uni-Kl.De/Pby3Z1Oeslyvlcipq_Iqug -
You'll Never Guess This Driving School Reviews's Tricks Driving School Reviews
Guide To Mazda Key Code: The Intermediate Guide For Mazda Key Code Mazda Key Code
You'll Never Be Able To Figure Out This Key Nissan's Benefits Key Nissan
High Quality Washer Dryer 101: This Is The Ultimate Guide For Beginners Günstiger Waschtrockner
See What UPVC Door Threshold Repair Tricks The Celebs Are Making Use Of UPVC Door Threshold Repair
You'll Be Unable To Guess Best Window Hinge Repairs's Benefits Best Window Hinge Repairs
10 Things That Your Family Teach You About Small Tandem Pushchair Small Tandem Pushchair
The 10 Most Scariest Things About ADHD In Adults Test ADHD In Adults Test
10 Reasons You'll Need To Know About Cordless Tools For Diyers Oberfräse FüHrungsschiene Set
Standing Compressor 50L Tips To Relax Your Daily Life Standing Compressor 50L Trick That Everyone Should Learn standing compressor 50l
Five Killer Quora Answers On Double Glazing Moisture Double Glazing Moisture
Guide To Replacement Key Fob Subaru: The Intermediate Guide To Replacement Key Fob Subaru Replacement Key Fob Subaru (https://md.entropia.de/)
A Provocative Rant About Electric Treadmills For Running electric Treadmill for Running
Five Killer Quora Answers To Fiat Ducato Key Replacement fiat ducato Key Replacement
Where Do You Think Loft Beds With Desk Be One Year From This Year? Bed with a desk (https://posteezy.com/ultimate-glossary-terms-about-bed-desk-under)
10 Things That Your Family Taught You About UPVC Frame Repair upvc frame repair (beauty-community.Com)
5 Killer Quora Answers To Window Refurbishment window Refurbishment
Do You Think You're Suited For Doing Dewalt Battery Operated Tools? Check This Quiz Dewalt Battery Tools
10 Double Glazing Installers Near Me Tricks All Pros Recommend local double glazing companies
5 Qualities That People Are Looking For In Every NAD+ Boosters Vs Mitophagy Activators mitolyn supplement Discount
Unexpected Business Strategies That Aided Replacement Mercedes Key Succeed Replacement mercedes key fob
Why We Our Love For Cot Bed Baby (And You Should Also!) tots and cots
Pain Relief Prescriptions Tools To Streamline Your Daily Lifethe One Pain Relief Prescriptions Trick That Every Person Must Be Able To Pain Relief Prescriptions
You'll Never Guess This White Wine Fridge's Tricks white Wine fridge
10 Things That Your Family Teach You About Replacement Ford Car Key Replacement Ford Car Key
The 12 Best Planing Machines Selection Accounts To Follow On Twitter Top-Hobelmaschinen
What's The Current Job Market For Coffee Maker Bean To Cup Professionals Like? coffee maker bean to cup
The 10 Most Scariest Things About Window Refurbishment Window Refurbishment
10 Top Facebook Pages Of All Time Presentation Display Case Buffetwaermer
Fireplace With Mantel: Myths And Facts Behind Fireplace With Mantel Electric Fireplace With Mantel (500Px.Com)
5 Killer Quora Answers On Best Coffee Beans For Bean To Cup UK Best Coffee Beans For Bean To Cup UK
How To Outsmart Your Boss On Gaskets Replacement Exterior Door Seals
10 Facts About Modern Adjustable Desks That Will Instantly Make You Feel Good Mood Visita la fuente
Integrated Cooker And Hob Tools To Streamline Your Daily Lifethe One Integrated Cooker And Hob Technique Every Person Needs To Know integrated cooker and hob
Comprehensive Guide To U Sofa U Sofas
7 Small Changes That Will Make A Big Difference With Your Replacement Key For Smart Car Smart Keys - https://skipper-reese-4.technetbloggers.de/undeniable-proof-That-you-need-smart-key-services,
7 Simple Secrets To Totally Rocking Your Smart Washing Machine With Wi-Fi Bauknecht Frontlader 8 Kg Mit Dampffunktion Test
9 Things Your Parents Teach You About Buy Amitriptyline Hassle-Free Buy Amitriptyline Hassle-Free (Https://Tuttle-Castro-2.Blogbright.Net/So-Youve-Bought-Amitriptyline-On-Sale-Online-Now-What-3F)
What's The Job Market For L Shape Sofas Professionals Like? L Shape Sofa
The Underrated Companies To Monitor In The UPVC Door Emergency Repair Industry UPVC Door Technician
How To Build Successful Bedside Cot Bed For Infants Strategies From Home Cot Bed Drawers
10 . Pinterest Account To Be Following Buy A Real Austrian Drivers License Österreichischer Führerscheinservice
You'll Never Guess This BMW X5 Key's Tricks BMW X5 Key [Nybookmark.Com]
10 Things That Your Family Teach You About Couches For Sale Near Me couches for sale near me
The Most Common Private Mental Health Care Debate Doesn't Have To Be As Black Or White As You Might Think Psychiatry Private Practice
The 10 Most Terrifying Things About Tools Online UK Tools Online UK
It's The One Porsche Key Fob Trick Every Person Should Know Porsche Fob
A Retrospective A Conversation With People About Emergency Break-In Repair 20 Years Ago board up services near me
10 Facts About Multi Pod Coffee Machine That Can Instantly Put You In A Good Mood Pod Coffee Machines
5 Killer Quora Answers On BMW Replacement Key Bmw Replacement Key
See What Ignition Lock Cylinder Repair Tricks The Celebs Are Making Use Of Ignition Lock Cylinder Repair, Https://sweeney-dodd.hubstack.net/,
The 10 Most Scariest Things About House Lockout Service House Lockout Service
The 10 Most Scariest Things About Angle Grinder Set Cheap angle Grinder Set cheap
7 Secrets About Cheap Chest Freezer Test Winner That Nobody Will Tell You Leise Kühl-Gefrier-Kombination
The 10 Most Terrifying Things About New Volvo Car Key New Volvo Car Key
5 Killer Quora Answers To Online ADHD Test UK Online ADHD Test UK
15 Gifts For The Supplements To Boost Mitochondria Lover In Your Life Cheap Mitolyn Supplement Online; grady-barry-3.hubstack.net,
Why Adding Buy Tools Online To Your Life Will Make All The Difference Elektrowerkzeug
What's The Job Market For Sash Window Restoration Company Professionals Like? Sash Window Restoration Company
Five Killer Quora Answers On Refrigerator With Wine Rack Refrigerator With Wine Rack (forum.finveo.world)
8 Tips For Boosting Your Professional Steroids Germany Game Authentische Steroide In Deutschland
The 10 Most Terrifying Things About Legal Irish Driving License Supplier Legal Irish Driving License Supplier (https://historydb.date/wiki/15_Reasons_You_Shouldnt_Ignore_Buy_Genuine_Irish_Drivers_License)
The 10 Scariest Things About ADHD Assessment UK Private adhd Assessment uk private
The Unknown Benefits Of Driving License Cost loja De CNH - wikimapia.org,
Is Patio Door Frame Repair The Greatest Thing There Ever Was? Home Patio Door Repairs
What's The Current Job Market For Foggy Window Repair Professionals? Foggy Window Repair
Guttering Solutions Tips To Relax Your Daily Life Guttering Solutions Trick That Every Person Should Be Able To Guttering Solutions
Five Killer Quora Answers To Stainless Steel American Fridge Freezer Stainless Steel American Fridge Freezer
10 Tips To Build Your Planing Machines On A Budget Empire Holzbearbeitungshobelmaschinen Online Kaufen
You Are Responsible For A FUXTEC Sweeper Budget? Twelve Top Ways To Spend Your Money güde kehrmaschine angebot (6068688.Xyz)
What's The Job Market For B1 ÖSD Professionals Like? B1 ÖSD
5 Killer Quora Questions On Stihl Chainsaw Price Husqvarna 445 II Test
What's The Current Job Market For House Lock Installation Professionals Like? House Lock Installation
Guide To Tilt And Turn Windows Repair Cost: The Intermediate Guide The Steps To Tilt And Turn Windows Repair Cost Tilt And Turn Windows Repair Cost
What's The Current Job Market For I Lost My Car Keys Nissan Professionals Like? i lost my car keys nissan
17 Reasons Not To Ignore Door Seals Magnetic Door Seals
Sofa Bed Options 10 Things I'd Love To Have Known Earlier most comfortable Couch (https://milsaver.com/)
7 Tricks To Help Make The Most Of Your Subaru Car Key Subaru Car Key Replacement
Mobile Window Doctor Tools To Help You Manage Your Everyday Lifethe Only Mobile Window Doctor Trick That Everybody Should Learn Mobile Window Doctor, onioncomma14.bravejournal.net,
You'll Never Guess This Dewalt Xr Tools's Secrets Dewalt Xr Tools
The 10 Most Terrifying Things About Portable Bedside Crib portable bedside crib [https://Md.chaosdorf.de]
See What Window Hinge Repair Diy Tricks The Celebs Are Utilizing Window Hinge Repair Diy
What's The Job Market For Co-Sleeper Crib Professionals? Co-Sleeper Crib
Buy Milling Machines With Worldwide Shipping Tips From The Best In The Business fräSmaschinen mit Weltweitem versand Kaufen [https://Kitchenanswershub.com/user/sproutrake25]
Five Killer Quora Answers On Bunk Beds For Adults UK Bunk Beds For Adults UK
Does Technology Make Conservatory Refurbishment Better Or Worse? Secure Window Locks - Https://--7Sbarohhk4A0Dxb3C.рф/User/Ashshare0/,
How Bunk Bed For Sale Changed My Life For The Better bunk beds for sale
Why Polish Drivers License Documents Is Fast Becoming The Hottest Trend Of 2024 Zakup Polskiego Prawa Jazdy
10 Things You Learned In Kindergarden That Will Help You With Freezer Energy Efficiency Class C Gefriertruhe Groß Preis
20 Questions You Must Always To Ask About Baby Cot Before You Purchase Baby Cot cheap baby cots For sale
Guide To Oven And Hobs: The Intermediate Guide For Oven And Hobs oven and hobs
5 Clarifications On U Shaped Sectional Sofa u-shaped sectional sofa
How L Shaped Sectional Sofa Altered My Life For The Better L-Shaped Sectional Sofas
7 Small Changes That Will Make A Big Difference In Your Best Baby Cot Best Baby Cots
10 Healthy Habits For A Healthy Polish License Fees Prawo Jazdy b
How To Explain Car Key To A Five-Year-Old Car Key Cutting
What's The Job Market For Electric Wall Mounted Fires Professionals Like? Electric Wall Mounted Fires
See What Home Treadmill With Incline Tricks The Celebs Are Utilizing Home Treadmill With Incline
Why U-Shaped Sofa Is Fast Becoming The Most Popular Trend For 2024 Couch Chaise
The 10 Most Terrifying Things About MDMA Online Legit mdma online legit
See What Baby Bed Cot Tricks The Celebs Are Making Use Of Baby Bed Cot
15 Top Pinterest Boards Of All Time About Glass Display Case warmhalter
10 Tips For Quickly Getting Battery Powered Grinder Best Angle Grinder Cordless
15 Twitter Accounts You Should Follow To Learn More About Window Hinges Window Hinge Repairs
15 Terms That Everyone Working In The Online Fridge Sale Industry Should Know Wärmepumpentrockner A+++ Günstig
45 Foot Shipping Containers Tools To Ease Your Daily Life 45 Foot Shipping Containers Trick That Everybody Should Know 45 foot Shipping containers
11 Ways To Completely Revamp Your Cordless Pole Pruner Chainsaw Nilfisk Hochdruckreiniger
The 3 Greatest Moments In Condensation In Windows History Window Condensation
Guide To L Shape Sofa: The Intermediate Guide On L Shape Sofa L Shape Sofa (cameradb.review)
Guide To Audi Key Lost: The Intermediate Guide To Audi Key Lost audi key lost
Ten Startups That Are Set To Change The Washing Machine Shop Industry For The Better Reduzierte Waschmaschinen Online
15 Reasons Why You Shouldn't Ignore Refrigerator With Wine Rack Wine Beer Fridge
You'll Be Unable To Guess Handmade Sofa Set's Secrets Handmade Sofa Set
You'll Be Unable To Guess Capsule Machine Coffee's Secrets Capsule Machine Coffee (notes.io)
The Steve Jobs Of Spanish Driving Licence Online Meet Your Fellow Spanish Driving Licence Online Enthusiasts. Steve Jobs Of The Spanish Driving Licence Online Industry Permiso de conducir español con entrega rápida, historydb.date,
The 10 Most Scariest Things About New BMW Key New BMW Key
The 10 Most Scariest Things About Mental Health Assesment Mental Health Assesment (Https://Whisperduneshoa.Com/)
You'll Never Be Able To Figure Out This Fiat Ducato Spare Key's Benefits Fiat Ducato Spare Key
Why Nobody Cares About Bedside Cot For Cribs Cotbed With Draw (Hackmd.Okfn.De)
10 Things You've Learned In Kindergarden To Help You Get Hyundai Car Key Hyundai Keys
Ten Triple Bunks That Really Make Your Life Better Triple Bunks
Ten Vw Replacement Keys That Really Change Your Life Vw Replacement Keys, Https://telegra.ph/,
20 Fun Facts About Walking Treadmill Self Powered Walking Treadmill
A Look In The Secrets Of Fiat 500 Replacement Key Fiat 500 Replacement Key Fob (intensedebate.com)
12 Companies That Are Leading The Way In Door Handle Troubleshooting Door handle Hardware repair (www.askocloud.com)
The Most Powerful Sources Of Inspiration Of Portable Bedside Crib Drawer Cot Bed
9 . What Your Parents Taught You About Buy Co Codamol On The Internet buy co codamol on the internet
20 Up-And-Comers To Watch In The Mobility Scooter To Buy Industry mobility scooters near me (Https://bookmarkingdelta.com/)
This Is What Sash Window Repairs Will Look Like In 10 Years Time Sash Window Repairs Near Me
14 Smart Ways To Spend Left-Over Goodyear Eagle F1 Summer Tires 225 45 R17 Deal Budget neue sommerreifen kaufen
Solutions To Issues With Automotive Key Automotive Key Locksmith
9 Things Your Parents Taught You About Broken Window Crank Handle Replacement Broken window crank handle replacement (http://cqr3d.ru)
14 Businesses Doing A Great Job At Rotten Conservatory Frames fixing window locks, Forum.issabel.Org,
The Most Common ADHD Test Online Mistake Every Beginning ADHD Test Online User Makes Online Adhd Testing (Clashofcryptos.Trade)
The Most Successful Drill Comparison Gurus Are Doing 3 Things Bohrhammer
The 10 Most Terrifying Things About 12v Circular Saw 12V Circular Saw
The 10 Most Scariest Things About Best Small Wine Refrigerator Best Small Wine Refrigerator [https://pads.jeito.nl/S/IJfOYVDdk]
See What Autofold Mobility Scooter Tricks The Celebs Are Utilizing autofold mobility scooter
It Is The History Of Grinding Machines Web Store In 10 Milestones Tragbare Schleifmaschinen online kaufen
Guide To Sash Window Services In My Area: The Intermediate Guide The Steps To Sash Window Services In My Area Sash Window Services In My Area [travelersqa.com]
9 Lessons Your Parents Taught You About Mental Health Diagnosis Private Mental Health Diagnosis Private
You'll Never Be Able To Figure Out This Panel Restoration Services's Tricks Panel Restoration Services
Unexpected Business Strategies That Helped Buy Goethe B1 Language Certificate Achieve Success goethe zertifikat b1 deutsch online Kaufen
Three Greatest Moments In Driving Instructors Grimsby History Driving School Grimsby
You'll Never Be Able To Figure Out This Luxury Window Handle Replacement's Secrets luxury Window Handle replacement
How You Can Use A Weekly Composite Door Handle Fix Project Can Change Your Life Local composite door Repairs
Begin By Meeting The Steve Jobs Of The Oven And Hob Industry Food Preparation
5 Killer Quora Answers On Black Window Handle Replacement Black Window Handle Replacement
Ten Myths About Polish Category C Driving License What Can You Drive That Aren't Always True Europejskie Prawo Jazdy Bez Egzaminu
How To Get Better Results Out Of Your Mini Cooper Replacement Key Replacement Mini Cooper Key (fakenews.win)
10 Healthy Height Adjustable Table Frames Habits Mesa De Escritorio De Altura Ajustable
Pay Attention: Watch Out For How Best Cot Is Taking Over And What You Can Do About It Large Travel Cot
Electric Fireplace Suites Tools To Ease Your Daily Life Electric Fireplace Suites Technique Every Person Needs To Know Electric Fireplace Suites (Bestbizportal.Com)
The 10 Most Scariest Things About Barista-Quality Sage Coffee Machines Barista-Quality Sage Coffee Machines (digitaltibetan.win)
9 . What Your Parents Taught You About Built In Electric Oven built in electric oven
The 10 Most Terrifying Things About French Door Refrigerator For Sale French Door Refrigerator For Sale (Notes.Io)
Be On The Lookout For: How Grinding Machines On The Web Is Gaining Ground, And What To Do Spitzenlose Schleifmaschinen Online Kaufen
What's The Current Job Market For Tilt And Turn Window Mounting Bracket Repair Professionals? Tilt And Turn Window Mounting Bracket Repair
Enough Already! 15 Things About Robotic Vacuum We're Fed Up Of Hearing Robot vacuum cleaner
See What Upvc Soffit Tricks The Celebs Are Utilizing Upvc Soffit
What's The Current Job Market For House Key Duplication Professionals? House Key Duplication
20 Trailblazers Are Leading The Way In Industrial Planing Machines hobelmaschinen-marken (https://pattern-wiki.win)
Nine Things That Your Parent Taught You About Key Fob For Lexus key fob for Lexus
Are You Responsible For The Cots To Tots Budget? 12 Ways To Spend Your Money Best cot for newborn
5 Killer Quora Answers To Glazing Repair Experts Glazing Repair Experts
Do Not Believe In These "Trends" Concerning Mental Health Test UK Book A Mental Health Assessment
The Top Reasons People Succeed With The Bosch Series 8 Oven Price Comparison Industry Siemens Waschmaschine Iq500
You'll Be Unable To Guess Window Draft Seals's Secrets Draft Seals
The Top Companies Not To Be In The Sweeper Offer Industry KettensäGe Online Bestellen
What's The Point Of Nobody Caring About Compare Washing Machine Prices Waschmaschinen-Lieferung (rant.li)
"The Ultimate Cheat Sheet" On 30 Foot Containers 30 Foot Shipping Container Cost
The 10 Most Scariest Things About Hyundai Extra Key Hyundai Extra Key
You Are Responsible For An Sectional U Shaped Budget? 12 Ways To Spend Your Money Chaise sofa
The People Closest To Portable Milling Machines Share Some Big Secrets Fräsmaschinen Zu Reduzierten Preisen Kaufen
See What Renault Key Card Replacement Near Me Tricks The Celebs Are Making Use Of Renault Key Card Replacement Near Me
5 Killer Quora Answers To Lost Car Keys Vauxhall Corsa Lost Car Keys Vauxhall Corsa
Guide To Mobility Scooters Near Me For Sale: The Intermediate Guide For Mobility Scooters Near Me For Sale Mobility scooters near me For sale
10 Healthy Buy Belgium Driving License Online Habits Goedkoop Belgisch Rijbewijs
What Is It That Makes Book ADHD Assessment So Famous? Cost Of Private ADHD Assessment UK
Buy Pain Relief Solutions Online Tools To Make Your Daily Life Buy Pain Relief Solutions Online Trick That Every Person Must Be Able To Buy Pain Relief Solutions Online
Fridge On Sale Tips That Will Change Your Life Refrigerator Sale
5 Killer Quora Answers On Cordless Nail Guns For Sale cordless Nail guns for Sale
Guide To Hyundai Car Keys: The Intermediate Guide The Steps To Hyundai Car Keys Hyundai Car Keys
The 9 Things Your Parents Taught You About Door Draft Stoppers Door Draft Stoppers
The Best Double Pushchairs Tricks To Make A Difference In Your Life best double pushchairs (https://md.un-hack-bar.de/ufacjqb-tcscyqficst3jq)
What's The Job Market For Jaguar Replacement Car Keys Professionals? Jaguar Replacement Car Keys
See What Double Glazed Window Repairs Tricks The Celebs Are Using Double Glazed Window Repairs
The 9 Things Your Parents Taught You About Roomba Self Empty Roomba Self Empty
The 10 Most Scariest Things About Cheap Coffee Machine UK coffee Machine uk (output.Jsbin.com)
20 Up And Coming Repairing Conservatory Doors Stars To Watch The Repairing Conservatory Doors Industry lock Troubleshooting
The 10 Scariest Things About Sash Window Fixer Nearby Sash Window Fixer Nearby
Five Killer Quora Answers On Fiat Replacement Key Fob Fiat Replacement Key Fob
5 Reasons To Consider Being An Online Fridge Buy And 5 Reasons You Shouldn't Online Fridge
7 Tips About Folding Treadmill With Incline That Nobody Will Share With You High Incline Treadmill
The 10 Scariest Things About Window Sash Repair Window sash Repair
14 Smart Strategies To Spend Extra ADHD Free Test Budget ADHD Test
See What L Shaped Couch Sectional Tricks The Celebs Are Using l shaped Couch sectional - bbs.161forum.com,
Guide To ADHD Test UK: The Intermediate Guide In ADHD Test UK ADHD Test UK
10 Electric Ovens Online Tips All Experts Recommend range
Guide To Replacement Ford Focus Key: The Intermediate Guide On Replacement Ford Focus Key Replacement Ford Focus Key
You'll Never Guess This House Lock Upgrade's Tricks House Lock Upgrade
15 Surprising Facts About Interactive Touch Display 4K Monitor FüR Business
The Hidden Secrets Of Advanced Electric Treadmills Electric Treadmill Reviews
What's The Current Job Market For Confidential Hacker Services Professionals Like? Confidential Hacker Services
12 Stationary Planer Facts To Refresh Your Eyes At The Water Cooler Cnc Fräse Einsteiger Set
Guide To Locksmith For Your House: The Intermediate Guide Towards Locksmith For Your House Locksmith For Your House
See What Best Headphones Online Shopping Tricks The Celebs Are Utilizing Best Headphones Online Shopping (https://md.chaosdorf.de/MvUiiiJ2T_uFL-eM1Uk93w)
10 Places That You Can Find Wooden Pallets Marketplace Find Wooden Pallets
10 Best Facebook Pages That I've Ever Seen. Door Knobs Repair door knob repair, Pad.stuve.uni-ulm.de,
Guide To Power Tools UK: The Intermediate Guide To Power Tools UK Power Tools UK (Telegra.Ph)
How To Save Money On 3 Wheel Pushchair 3 Wheel Pushchairs (Hslife.deegao.com.cn)
10 Mistaken Answers To Common Lexus Key Fob Questions: Do You Know The Right Ones? lexus key Fob Replacement
What Norwegian Driving License Cost Experts Want You To Learn Rimelig Norsk Førerkort
Why Nobody Cares About Dewalt Tool Set dewalt Tool sets
You'll Be Unable To Guess Bedside Cot For Experienced Parents's Benefits Bedside Cot For Experienced Parents (Md.Chaosdorf.De)
You'll Never Be Able To Figure Out This Table Mitre Saw's Tricks table Mitre saw
15 Shocking Facts About Who Repairs Sliding Patio Doors Sliding Patio Door Replacement
See What 3 Wheeler Off Road Buggy Tricks The Celebs Are Using 3 Wheeler Off Road Buggy
What's The Job Market For Citroen C4 Key Replacement Professionals? citroen c4 Key Replacement
How To Tell If You're Prepared To Go After Double Glazing Cost Local installation company
9 Things Your Parents Teach You About Co Codamol Online Delivery Co Codamol Online Delivery
Who Is Responsible For The Buy A Cheap Freestanding Hob Budget? 12 Tips On How To Spend Your Money Einbaubackofen Test
How To Become A Prosperous Comfy Sofas For Sale Entrepreneur Even If You're Not Business-Savvy Affordable Couches For Sale, Https://Output.Jsbin.Com/Wucifoxave/,
14 Misconceptions Commonly Held About Washer Dryer Combo Discount Beste Waschtrockner, Cameradb.review,
How To Outsmart Your Boss On Site To Buy Cnh Comprar Carta de Condução da Categoria B1 [moparwiki.win]
Get To Know You The Steve Jobs Of The Private ADHD Assessment Bedford Industry Private adhd assessment wales cost
5 Killer Quora Answers On Replacement Land Rover Key Replacement Land Rover Key
What's The Job Market For House Lock Changing Professionals? House lock Changing
What's The Job Market For Pull Out Bed Couches Professionals? Pull Out Bed Couch
A Provocative Rant About Patio Door Lock Repair Patio Door Hinge Repair
What Is The Reason? Hob With Extractor Hood Comparison Is Fast Becoming The Hot Trend For 2024? Induktionskochfeld Rahmenlos Angebot
See What Replacement Key For Peugeot 107 Tricks The Celebs Are Utilizing Replacement Key For Peugeot 107
Citroen Key Cutting Techniques To Simplify Your Daily Lifethe One Citroen Key Cutting Trick That Should Be Used By Everyone Be Able To Citroen Key Cutting
What's The Job Market For Citroen Replacement Key Professionals Like? Citroen replacement key
9 Lessons Your Parents Teach You About Electric Wall Mount Fireplace Electric Wall Mount Fireplace (http://Www.Uk-corp.co.uk/)
20 Fun Facts About Fridge Freezer Online Wärmepumpentrockner Kaufen
The Top Reasons Why People Succeed In The Orbital Sander With Dust Extraction Industry Akku Schlagschrauber Hohes Drehmoment
20 Inspiring Quotes About Online Psychiatrist Private Psychiatry Practice
What Is The Reason Why Mitolyn Supplement Official Website Are So Helpful During COVID-19 Mitolyn Supplement For Sale
5 Killer Quora Answers On 1kg Coffee Beans For Coffee Lovers 1kg Coffee Beans For Coffee Lovers
Buzzwords De-Buzzed: 10 Different Methods To Say Purchasing Finnish Driver's License Kuinka Ostaa Suomalainen Ajokortti
20 Reliable Pressure Washer Online Websites Taking The Internet By Storm Top-Angebote Für Hochdruckreiniger (mindwellnessforum.com)
A Delightful Rant About Cordless Nailer Set Deals Dickenhobel Hobelmaschine testsieger
20 Damaged Window Hinge Repair Websites Taking The Internet By Storm Aluminum Window Hinge Repairs
What's The Current Job Market For Mazda Spare Key Cost Professionals? Mazda Spare Key
The 10 Most Scariest Things About Misted Glass Repair Misted glass Repair
What's Holding Back What's Holding Back The Incline Treadmills Industry? Adjustable Incline Treadmills
What Freud Can Teach Us About Saab Key Programming Saab key programming near me
Guide To Sash Window Services In My Area: The Intermediate Guide On Sash Window Services In My Area sash window Services in my area
10 Ways To Create Your Baby Cot Empire travel cot uk (covolunteers.com)
What Is Warming Box And How To Use It Warmhaltekoffer (swaay.com)
Guide To Mitsubishi Lancer Key Fob: The Intermediate Guide On Mitsubishi Lancer Key Fob Mitsubishi lancer Key
You'll Never Be Able To Figure Out This Window Hinge Maintenance Tips's Tricks window hinge maintenance
The 10 Most Terrifying Things About Bunk Beds Near Me bunk Bed
The 10 Most Terrifying Things About Bedside Cot For Travel Bedside Cot For Travel
Honda Replacement Key UK Tools To Ease Your Daily Lifethe One Honda Replacement Key UK Trick That Everybody Should Know Honda Replacement Key UK (Forum.Ceoiam.Com)
Who's The Top Expert In The World On Guttering Installation? Downspouts
The History Of Router Comparison In 10 Milestones Oberfräse füHrungsschiene set
10 Things That Your Family Teach You About Counterfeit Money Websites Counterfeit Money Websites
See What Espresso Maker Tricks The Celebs Are Utilizing Espresso Maker
See What Wheelchair Foldable Lightweight Tricks The Celebs Are Utilizing wheelchair foldable Lightweight
You'll Be Unable To Guess Tilt And Turn Window Handle Replacement's Tricks Tilt And Turn Window Handle Replacement
20 Best Tweets Of All Time About Double Pram Tandem Pram
The Most Valuable Advice You Can Receive About Window Doctor Custom Window Doctor
See What Buy Coffee Beans In Bulk Tricks The Celebs Are Using Coffee Beans In Bulk
Guide To Original UK Drivers License: The Intermediate Guide To Original UK Drivers License Original UK Drivers License (bossen-deleuran-2.hubstack.net)
A Trip Back In Time What People Said About Headphone Buy Online 20 Years Ago Quality Headphones
What's The Most Creative Thing That Are Happening With Pneumatic Combination Nailer Reviews elektrotacker für Holz
What Are The Myths And Facts Behind Hacking Services Ethical Hacking Services [Https://cameradb.review/]
The Advanced Guide To Fake Driving License schweizer Fahrerlaubnis
5 Killer Quora Answers To Tilt And Turn Window Replacement Parts tilt and turn window replacement parts
15 Best Pinterest Boards Of All Time About Test For ADHD Test For ADHD Online
Repair Broken Tilt And Turn Windows Tools To Improve Your Daily Lifethe One Repair Broken Tilt And Turn Windows Technique Every Person Needs To Know Repair Broken Tilt And Turn Windows
Guide To Pushchairs Shop: The Intermediate Guide To Pushchairs Shop pushchairs Shop
The Best Robot Vacuum And Mop Self Empty Tricks To Change Your Life best Robot vacuum and mop self Empty
Robot Vacuum Self Emptying Techniques To Simplify Your Daily Lifethe One Robot Vacuum Self Emptying Trick That Should Be Used By Everyone Know Robot Vacuum Self Empty (https://petersen-hjelm-2.hubstack.net)
Are You Responsible For A House Locksmith Company Budget? Twelve Top Tips To Spend Your Money House Locksmith Services
12 Facts About Bedside Cot For Parents To Make You Think About The Other People Cot And Drawers
Cheap Drill: A Simple Definition Bohrmaschine Online Bestellen
What Is Headphones Sale UK And Why Is Everyone Speakin' About It? Headphone Sales
17 Signs You Are Working With Good Sweepers Kehrmaschinen Mit ZubehöR - Bbs.Xingxiancn.Com -
10 Places Where You Can Find Mercedes Replacement Key Mercedes Replacement Key Cost
This Is The One Danish License Agent Trick Every Person Should Know Bestil Dansk KøRekort
The 10 Most Dismal B1 Exam Costs Failures Of All Time Could Have Been Prevented leben in deutschland zertifikat kaufen
The Reasons You're Not Successing At Latest Washing Machines Frontlader-Waschmaschine online kaufen (yogaasanas.science)
What's The Job Market For Peugeot 107 Key Replacement Professionals? Peugeot 107 key
The 10 Scariest Things About Conservatory Roof Repair conservatory roof repair
An Easy-To-Follow Guide To Buy Height Adjustable Desks Online Conversores De Escritorios De Pie Ajustables
How To Create Successful Buy A Fridge Instructions For Homeschoolers From Home Bester Waschtrockner Stiftung Warentest
How To Get More Results Out Of Your Jaguar Car Key jaguar car Keys
7 Small Changes That Will Make A Huge Difference In Your Broken Door Repair Composite door Repair Contractors
You'll Be Unable To Guess Best Mitochondrial Support Supplement's Benefits Best mitochondrial Support supplement
10 Facts About Heavy-Duty Compressor Purchase That Can Instantly Put You In An Optimistic Mood Gewerbekompressor Online Kaufen
10 Graphics Inspirational About Peugeot Car Keys Replacements Peugeot Car Key Replacement (https://bestbizportal.com/)
12 Facts About ADHD Test Free To Make You Think Twice About The Cooler Water Cooler Free Online ADHD Test (https://pad.geolab.space)
Question: How Much Do You Know About Cheap Fridge Freezer Online? Unterbaufähige waschmaschine kaufen
An In-Depth Look Back What People Talked About Upvc Panel Restoration 20 Years Ago Panel Replacement - https://www.tomahawknation.com -
9 Lessons Your Parents Taught You About ADHD Online Test UK ADHD Online Test UK
Five Killer Quora Answers On Manual Treadmill Non Electric Manual Treadmill Non Electric
You'll Never Guess This ADHD Diagnosis Test's Tricks ADHD Diagnosis Test
Five Killer Quora Answers To Fridges To Buy Fridges To Buy
Guide To UPVC Door Repair Service Near Me: The Intermediate Guide On UPVC Door Repair Service Near Me upvc door repair service near me
Petrol Sweeper With Self-Propulsion Tools To Ease Your Daily Lifethe One Petrol Sweeper With Self-Propulsion Trick That Every Person Must Be Able To Petrol Sweeper With Self-Propulsion
The Getting A Polish Drivers License Success Story You'll Never Remember Informacje O Polskim Prawie Jazdy
10 Things You Learned In Kindergarden Which Will Help You With Best Pod Coffee Machine UK Pod Coffee Machines
Five Killer Quora Answers To Fiat Replacement Key Fob Fiat Replacement Key Fob
The Biggest Sources Of Inspiration Of Buy Certificate zertifikat Telc B1
Five Killer Quora Answers On Seat Ibiza Spare Key Seat Ibiza Spare Key
20 Tools That Will Make You More Effective At Planing Machines Offers Hobelmaschinen-Typen
What Is Reliable Window Hinge Repairs? Heck Is Reliable Window Hinge Repairs? Common Window Hinge Problems (www.xsmoli.com)
A Help Guide To U Sectional Couch From Beginning To End U Sectionals
See What Gaskets Replacement Tricks The Celebs Are Making Use Of Gaskets Replacement
The 10 Most Scariest Things About Mazda Car Key Replacement Cost Mazda Car Key Replacement
You'll Never Be Able To Figure Out This Cheapest Chest Freezers's Tricks Cheapest Chest Freezers
20 Trailblazers Setting The Standard In Emergency Window Repair Window Replacement (https://humanlove.stream/wiki/What_Freud_Can_Teach_Us_About_Window_Restoration)
What's The Current Job Market For Battery Skill Saw Professionals? Battery Skill Saw
What Is Pneumatic Nailer Reviews And Why Are We Talking About It? Profi werkzeug online bestellen
5 Best Lightweight Mobility Scooter Uk Myths You Should Avoid Mobility scooter Stores
You'll Never Guess This Sash Window Replacement Specialists's Tricks sash window replacement specialists
You'll Never Guess This 24-Hour House Locksmith's Tricks 24-hour House locksmith (https://nicolajsen-tyson-3.blogbright.net/)
The 10 Most Terrifying Things About Best Rated Folding Treadmill Best Rated Folding Treadmill
Ask Me Anything: 10 Responses To Your Questions About Conservatory Maintenance window lock specialists
What's The Job Market For Buy Lighting UK Professionals Like? buy Lighting uk
20 Trailblazers Leading The Way In Sofa L Shape Sofa l'shape, 114.67.155.184,
This Is The Intermediate Guide In Wine Fridges wine Coolers uk
House Lock Security Tools To Help You Manage Your Everyday Lifethe Only House Lock Security Trick That Every Person Should Learn House Lock Security
Who Is 60 Cm Wide Dishwasher Comparison And Why You Should Care GeschirrspüLer Einbau Angebot
The 9 Things Your Parents Taught You About Oven Integrated Oven integrated
9 . What Your Parents Teach You About Broken Window Crank Handle Replacement Broken Window Crank Handle Replacement
Tumble Dryers In Stock: 11 Thing You're Forgetting To Do Günstige HaushaltsgeräTe
How The 10 Worst L Shape Couches FAILS Of All Time Could Have Been Prevented L-Shape Couch
10 Things We Love About Best Place To Buy Goethe B1 B1 Deutsch Prüfung Online Kaufen
What's The Job Market For Fully Integrated Dishwasher Affordable Professionals Like? Fully Integrated Dishwasher Affordable
Learn About Order Router Online While Working From At Home Dickenhobel Maschine Preisvergleich
U Sectional Couch Tools To Make Your Daily Life U Sectional Couch Trick Every Person Should Know U Sectional Couch (Lanier-rowe-5.blogbright.net)
20 Resources To Make You More Efficient With Baby Cotbed Wooden Cotbed
What's The Current Job Market For Medical 3 Wheel Scooter Professionals? medical 3 wheel scooter
You'll Be Unable To Guess BMW Key Lost's Tricks BMW Key Lost
How To Create An Awesome Instagram Video About Buy Height Adjustable Desks Online Escritorio eléctrico de altura ajustable
See What House Rekey Service Tricks The Celebs Are Using House Rekey Service
Where Can You Find The Top Patio Door Repairs Information? Patio Door Threshold Repair
See What Buy Amitriptyline Without Prescription Tricks The Celebs Are Using Buy Amitriptyline Without Prescription; https://Sciencewiki.science/wiki/Ten_Startups_That_Will_Revolutionize_The_Buy_Generic_Amitriptyline_Online_Industry_For_The_Better,
Buy Washing Machine With Warranty's History Of Buy Washing Machine With Warranty In 10 Milestones HaushaltsgeräTe Online Kaufen
What To Focus On When Making Improvements To Compact Washing Machines Top-Angebote füR Waschmaschinen
What's The Job Market For Standard Tilt And Turn Window Repair Cost Professionals Like? Standard Tilt And Turn Window Repair Cost
Guide To Bedside Cot For Parents: The Intermediate Guide For Bedside Cot For Parents Bedside Cot For Parents
Guide To Goethe C2 Certificate: The Intermediate Guide For Goethe C2 Certificate Goethe c2
Guide To Delonghi Espresso Machines: The Intermediate Guide Towards Delonghi Espresso Machines Delonghi Espresso Machines
How To Explain L Shape Sectional To A 5-Year-Old L Couches (https://www.footballzaa.com/out.php?Url=https://www.sofasandcouches.com/products/beige-modern-l-shaped-sectional-sofa-with-ottoman)
Do Not Believe In These "Trends" About Polish Driving License Process Koszt Polskiego Prawa Jazdy
Subaru New Key Tools To Improve Your Everyday Lifethe Only Subaru New Key Trick Every Individual Should Learn Subaru New Key
What's The Job Market For Saab 9-3 Key Replacement Professionals Like? Saab 9-3 Key Replacement
Guide To ADHD Test Free: The Intermediate Guide For ADHD Test Free Adhd Test Free
Your Worst Nightmare Concerning Preventing Conservatory Leaks Be Realized Lock Repair Services
Guide To Renault Car Key: The Intermediate Guide For Renault Car Key Renault Car Key
Ten Reasons To Hate People Who Can't Be Disproved Quiet Sweepers Kehrmaschinen FüR Zuhause
The 10 Most Scariest Things About ADHD Assessment Test ADHD Assessment Test
Guide To UPVC Door Draught Repair: The Intermediate Guide In UPVC Door Draught Repair UPVC Door Draught Repair
Online Test For ADHD Tools To Streamline Your Daily Lifethe One Online Test For ADHD Technique Every Person Needs To Be Able To Test For ADHD (kanban.xsitepool.tu-freiberg.de)
See What Smart Car Door Lock Tricks The Celebs Are Making Use Of Smart Car Door Lock (Hack.Allmende.Io)
7 Useful Tips For Making The Most Of Your Buy A2 Driver's License Online Führerschein Online Drucken
What Are The Myths And Facts Behind Buy Counterfeit Money On The Darknet Legal Falschgeld Darknet; diigo.Com,
You'll Be Unable To Guess Couch U Shape's Tricks Couch U Shape
See What ADHD Online Test Adults Tricks The Celebs Are Utilizing adhd Online test adults
Are You Responsible For An Auto Key Budget? 10 Fascinating Ways To Spend Your Money Replacement Auto Keys
Five Killer Quora Answers To Vw Lost Key Vw Lost Key
Five Killer Quora Answers On Wall Mount Electric Fire Place Wall Mount Electric Fire Place
15 Things You're Not Sure Of About American Fridge Freezer American Fridge Freezer Ice Dispenser
See What Automatic Vacuum Cleaner And Mop Tricks The Celebs Are Utilizing automatic vacuum Cleaner
Guide To Window Caulking: The Intermediate Guide The Steps To Window Caulking Window Caulking
The 10 Most Scariest Things About Citroen Key Genuine Citroen key fob replacement
What's The Current Job Market For Roomba Self Emptying Professionals Like? roomba Self Empty
Why All The Fuss Over ADHD Test For Adults? adhd test for adults free
20 Things You Should Know About Window Sash Repair Best window repair company
Are You Able To Research Versatile Impact Wrench Online Schlagschrauber-Kit
9 . What Your Parents Teach You About Patio Door Repairs Near Me Patio Door Repairs Near Me
Nine Things That Your Parent Taught You About Tilt And Turn Window Exterior Repair Tilt And Turn Window Exterior Repair
What's The Job Market For Electric Folding Wheelchair For Sale Professionals Like? Electric Folding Wheelchair
11 Creative Methods To Write About Angle Grinder Brushless brushless angle grinder
Are You Getting The Most Of Your Cot Bed Sale? Cot Beds
Guide To All Terrain Travel System: The Intermediate Guide In All Terrain Travel System All terrain travel system
10 Things That Everyone Is Misinformed About The Word "Bedside Crib For Small Spaces" Sleigh Cot Bed With Drawer
See What Wine Chiller Fridge Tricks The Celebs Are Using Wine Chiller Fridge
10 Reasons You'll Need To Be Aware Of Skoda Replacement Key Skoda Replacement Key Cost
The 10 Most Terrifying Things About Cheap Coffee Makers Online cheap coffee makers online - https://pilegaard-emborg.Federatedjournals.com/ -
See What Vacuum Robot Self Empty Tricks The Celebs Are Making Use Of Vacuum Robot self empty
How Reliable Glass Repair Became The Hottest Trend Of 2024 professional glass Repair (ai-db.Science)
Guide To 3 Wheel Jogger Stroller: The Intermediate Guide To 3 Wheel Jogger Stroller 3 Wheel Jogger Stroller
Guide To Brushless Angle Grinder: The Intermediate Guide For Brushless Angle Grinder Brushless Angle Grinder
Guide To Best 305mm Mitre Saw: The Intermediate Guide On Best 305mm Mitre Saw best 305mm mitre saw
Check Out: How Patio Door Repairs Is Taking Over And What Can We Do About It Patio Door Weatherstripping Repair [md.un-hack-bar.de]
A Relevant Rant About Citroen C3 Car Key citroen Key replacement near me - https://citroen-c4-key-fob-replac74073.wikiconverse.com/6092755/five_people_you_must_know_in_the_citroen_berlingo_van_key_fob_not_working_industry -
You'll Never Guess This Cat Door Contractor's Secrets Cat Door Contractor
A Cot Beds For Sale Success Story You'll Never Believe travel cot Bed
The 10 Most Terrifying Things About Buy A Cordless Angle Grinder Buy A Cordless Angle Grinder
The Reason Everyone Is Talking About Non Motorised Treadmill This Moment folding manual treadmill
You'll Never Be Able To Figure Out This Buy Driver License Online's Tricks Buy Driver License
What's The Point Of Nobody Caring About Bedside Crib For Small Spaces Cot With Drawer Storage (www.askmeclassifieds.com)
5 Lessons You Can Learn From Warming Container BuffetküHlvitrine
20 Best Tweets Of All Time About Delonghi Coffee Machines De'longhi Coffee Machines
A Glimpse Into Power Tools's Secrets Of Power Tools bohrhammer
You'll Never Guess This Window Emergency Service's Secrets Window Emergency Service
What's The Job Market For House Locksmith Services Professionals? house locksmith
5 Killer Quora Answers To Best Ovens Uk Best ovens uk
Renault Zoe Emergency Key Replacement Tools To Help You Manage Your Daily Lifethe One Renault Zoe Emergency Key Replacement Technique Every Person Needs To Know Renault Zoe Emergency Key Replacement (Https://Hedgedoc.Info.Uqam.Ca/FiIdRgx5Rrm9-UVGZV8I7G)
Guide To Subaru Replacement Key Services UK: The Intermediate Guide In Subaru Replacement Key Services UK Subaru replacement key Services uk (https://fkwiki.win)
Buzzwords De-Buzzed: 10 Alternative Ways Of Saying Hyundai Replacement Car Keys Replacement Hyundai Key
8 Tips To Up Your Impact Wrench Game Schlagschrauber
Guide To Tilt And Turn Window Mechanism Repair: The Intermediate Guide Towards Tilt And Turn Window Mechanism Repair Tilt And Turn Window Mechanism Repair
5 Killer Quora Answers On 30 Ft Shipping Container 30 Ft Shipping Containers
The Reason Why Storage Containers Is The Main Focus Of Everyone's Attention In 2024 Cargo Storage Containers
"Ask Me Anything": Ten Responses To Your Questions About Small Washer Dryer Die beste Waschtrockner-Kombination (hedge.fachschaft.informatik.uni-kl.de)
Fixing Conservatory Leaks Techniques To Simplify Your Daily Life Fixing Conservatory Leaks Trick That Every Person Must Learn Fixing conservatory leaks
The Reasons To Focus On Improving Triple Sleeper Bunk triple Sleeper bunk bed
10 Reasons You'll Need To Be Aware Of Electric Planing Machines Industriehobelmaschinen
Ten Common Misconceptions About Best Value Washing Machines That Aren't Always The Truth Bestbewertete Waschmaschinen
The 10 Scariest Things About Renault Zoe Emergency Key Replacement UK Renault Zoe Emergency Key Replacement UK
Why Cheap Integrated Oven Is More Difficult Than You Think electric Ovens built In
9 Lessons Your Parents Taught You About Skoda Citigo Key Replacement Skoda Citigo Key Replacement
The Best Twin Pushchairs Tricks To Change Your Life best Twin pushchair (https://Forum.Finveo.world)
See What Black Built-In Oven Tricks The Celebs Are Utilizing Black Built-In Oven
What's The Current Job Market For Private ADHD Assessment Adults Professionals? private adhd assessment adults
Five Killer Quora Answers To MItolyn Usa Mitolyn Usa
ADHD Psychiatrist Tips To Relax Your Daily Lifethe One ADHD Psychiatrist Trick That Everybody Should Know adhd psychiatrist
Window Hinge Troubleshooting Tools To Help You Manage Your Daily Life Window Hinge Troubleshooting Trick That Every Person Should Know Window Hinge Troubleshooting
Order Counterfeit Money On The Darknet Tips That Will Transform Your Life Falschgeld darknet marktplatz
15 Interesting Hobbies That Will Make You More Effective At Sash Window Repair Quotes Sash Window Repair Experts (https://Www.silverandblackpride.Com/users/lzsoz38)
Guide To Buy Unique Handmade Settee: The Intermediate Guide For Buy Unique Handmade Settee buy unique handmade settee
Guide To Saab Replacement Key Programming: The Intermediate Guide For Saab Replacement Key Programming saab replacement key Programming (https://notes.io)
A Time-Travelling Journey What People Said About Sliding Patio Door Repair Service 20 Years Ago Sliding Patio Door Replacement
10 Times You'll Have To Learn About Mini One Replacement Key Fob Mini One Key
Guide To Window Gasket Seals: The Intermediate Guide In Window Gasket Seals gasket seals (md.Chaosdorf.de)
Three Reasons Why 3 Reasons Why Your Goethe Certificate Is Broken (And How To Fix It) Zertifikat goethe institut (squareblogs.Net)
20 Quotes That Will Help You Understand Intensive Driving Grimsby Driving Schools In Grimsby
15 Best Coffee Beans 1kg Bloggers You Must Follow Best Coffee Beans 1kg
Bariatric Wheelchairs Tools To Help You Manage Your Daily Lifethe One Bariatric Wheelchairs Technique Every Person Needs To Learn Bariatric Wheelchairs
See What 3 Wheel Mobility Cart Tricks The Celebs Are Making Use Of 3 Wheel Mobility Cart
15 Best Door Locks Replacement Bloggers You Need To Follow best door locks Replacement
10 Things That Your Family Teach You About Electric Wall Mount Fireplace Electric Wall Mount Fireplace
5 Myths About Wooden Cot That You Should Stay Clear Of Solid Wood Cot Bed Uk
Quiet Fridge-Freezer Combination Tools To Help You Manage Your Everyday Lifethe Only Quiet Fridge-Freezer Combination Technique Every Person Needs To Know Quiet Fridge-Freezer Combination
10 Things Everybody Has To Say About U Shaped Sectional With Chaise U Shaped Sectional With Chaise sectionals with chaise
5 Killer Quora Answers On Soffit And Fascia Services soffit And fascia services
Wooden Bunk Beds With Slide Tools To Ease Your Everyday Lifethe Only Wooden Bunk Beds With Slide Trick That Should Be Used By Everyone Learn Wooden Bunk Beds With Slide
20 Trailblazers Leading The Way In Buy Counterfeit Money Online Where To Buy Counterfeit Money Online
10 Facebook Pages That Are The Best Of All Time Prams Baby Pram [Https://Hay-Hollis.Federatedjournals.Com/The-Worst-Advice-Weve-Received-On-Prams-Pushchairs]
You'll Never Be Able To Figure Out This Robot Vacuum Self Empty's Tricks Robot Vacuum Self Empty
9 Things Your Parents Taught You About Upvc Window Handle Replacement Upvc Window Handle Replacement
The 9 Things Your Parents Taught You About Weatherproofing Seals Weatherproofing seals
3 Wheeler Travel System Tools To Make Your Daily Lifethe One 3 Wheeler Travel System Trick That Should Be Used By Everyone Know 3 Wheeler Travel System (rant.li)
Are You Getting The Most From Your Cot Beds For Sale? best Crib newborn - bookmarkswing.com,
How Cheap Coffee Machine Online Changed My Life For The Better cheap coffee machines Online
15 Cot Sale Benefits That Everyone Should Be Able To Baby Cot
What's The Job Market For Tassimo Brewer Professionals Like? tassimo brewer - https://sundaynews.Info/user/hyenacarbon89/ -
The 10 Scariest Things About Dulco Coffee Machine Dulco coffee machine
Five Killer Quora Answers To Designer Window Handle Replacement Designer Window Handle Replacement
You'll Never Guess This Rechargeable Angle Grinder's Tricks rechargeable Angle grinder
Get To Know You The Steve Jobs Of The Buying Drugs Online Legally Industry Buy drugs Online
Why Washer Dryer Combo Deals Is More Difficult Than You Think Rabatt für Waschtrockner-Kombinationen
See What Robot Vacuum Cleaner Auto Empty Tricks The Celebs Are Utilizing Robot Vacuum Cleaner Auto Empty
Buy Adjustable Standing Desks Tips From The Top In The Business mesa de escritorio eléctrica de altura ajustable
Why Is Bedside Cot For Close Bonding So Famous? Cot Bed With Mattress And Drawer
You'll Never Guess This Bedside Cot For Infants's Tricks Bedside Cot For Infants
See What Mazda 3 Key Replacement Tricks The Celebs Are Using Mazda 3 key Replacement
10 Simple Steps To Start The Business Of Your Dream 18V Cordless Demolition Hammer Business schutzgas Schweißgerät günstig
What's The Job Market For Exquisite Handmade Sofa Professionals? Exquisite Handmade Sofa
The Most Common Replacement Mitsubishi Key Mistake Every Beginner Makes Replacement Mitsubishi Key Fob
10 Places To Find Peugeot Partner Key peugeot partner key replacement
The Three Greatest Moments In Ford Car Keys History ford car key replacement
Conservatory Door Repair Tools To Help You Manage Your Daily Lifethe One Conservatory Door Repair Trick That Every Person Should Be Able To conservatory Door Repair
You'll Never Guess This Sash Window Repairs's Secrets Sash Window Repairs
The 3 Largest Disasters In Induction Hob Comparison The Induction Hob Comparison's 3 Biggest Disasters In History Geschirrspüler Vollintegriert Erfahrungen (Directoryquick.com)
The 10 Scariest Things About Weather Seal Replacement Weather seal replacement
What UPVC Door Specialist Experts Want You To Be Educated upvc doors
What To Focus On When The Improvement Of Private ADHD Assessment Near Me adult adhd assessment private
5 Killer Quora Answers To Buy Drivers License Online buy drivers license online
Don't Be Enticed By These "Trends" Concerning Replacement Vw Car Key Replacement Vw Car Keys
Why Nobody Cares About Test For ADHD Online ADHD Test Online
You'll Never Guess This Fixing Conservatory Damage's Benefits fixing conservatory damage
10 Quick Tips On Best Deals On Washing Machines Waschmaschinen-Shop
5 Killer Quora Answers To Refrigerator French Door Refrigerator French Door
5 Laws That Will Help The Private Psychiatrist Industry find a Private Psychiatrist
10 Things You Learned In Kindergarden Which Will Aid You In Obtaining Buy Impact Wrench With Fast Shipping Schlagschrauber online Kaufen
9 . What Your Parents Teach You About UPVC Door Professional upvc door Professional
The 9 Things Your Parents Teach You About Mitolyn Sale mitolyn
You'll Never Be Able To Figure Out This Online Pharmacy USA's Secrets Online Pharmacy Usa
15 Top Fridge Online Bloggers You Should Follow top fridge - hedgedoc.eclair.ec-lyon.fr,
Why No One Cares About Window Frame Seals window seals
What's The Job Market For Natural Wood Cot Professionals Like? Natural Wood Cot
Are You Getting The Most The Use Of Your Getting A Polish Drivers License? dokumenty polskiego prawa jazdy (www.pradaan.org)
How Do You Explain Buy A2 Driving License Online To A Five-Year-Old A2 Führerschein Digital [https://posteezy.Com]
The 9 Things Your Parents Taught You About Conservatory Improvement Conservatory Improvement (Www.Giveawayoftheday.Com)
Your Family Will Be Thankful For Having This Wall Fires Electric Wall Fires, https://hack.allmende.io/4A-4qqMNTXSS8gP9fGjJJg,
The Reason Everyone Is Talking About Buy Sit Stand Workstations Right Now Estaciones De Trabajo Ajustables Para Trabajar De Pie (cameradb.review)
15 Up-And-Coming All Terrain Travel System Bloggers You Need To Watch best all terrain travel system (Https://pad.stuve.uni-ulm.de)
You'll Never Guess This Mercedes Key Specialist's Tricks Mercedes Key Specialist
10 Things That Your Family Taught You About Wine Rack Fridge Wine Rack Fridge - Https://Onlinevetjobs.com/author/trampcoin5 -
How To Build Successful Double Glazing Installers Near Me Strategies From Home find local double glazing installation
17 Signs To Know If You Work With Cot Bed Sale best rated cribs (Directory-king.com)
10 Erroneous Answers To Common Counterfeit Money Statistics Darknet Questions Do You Know The Correct Ones? Falschgeld Handel Darknet
How Much Can Bedside Cot Beds Experts Earn? Cot Drawer
What's The Current Job Market For 3 Wheel Scooter With Seat Professionals? 3 wheel scooter with seat
Then You've Found Your Wheelchair Ramps ... Now What? Lightweight Wheelchair Ramps
See What Window Inspection Tricks The Celebs Are Making Use Of Window Inspection
See What Energy Efficient Chest Freezer Tricks The Celebs Are Using energy efficient Chest freezer
How To Research Best Couches UK Online Couch in uk
So You've Bought UPVC Door Emergency Repair ... Now What? UPVC Door Technician
Broken Window Hinge Replacement Tools To Help You Manage Your Daily Life Broken Window Hinge Replacement Trick That Everyone Should Know Broken Window Hinge Replacement
11 "Faux Pas" Which Are Actually OK To Create Using Your Wooden Baby Crib Wooden crib
15 Presents For The L Shape Sofa Lover In Your Life Sofa L (https://schoolido.lu/user/congospot92)
Undeniable Proof That You Need Single Trip Containers 20Ft Container
Fixing Conservatory Leaks Tips That Will Transform Your Life window maintenance (askmotopros.com)
What's The Job Market For All Terrain Buggy UK Professionals? All Terrain Buggy UK
Don't Make This Silly Mistake With Your Sectional Couches sectional comfy sofa (https://pads.jeito.nl/cslIQxPWQH62fOVhzaC4MQ)
Five Killer Quora Answers To De Longhi de longhi
Slide Out Sofa Tools To Improve Your Daily Lifethe One Slide Out Sofa Trick Every Individual Should Learn Slide Out Sofa
5 Laws That Will Help The Rotten Conservatory Frames Industry lock Replacement (graph.Org)
Ford Key Tips From The Top In The Industry ford key Cutting
Why You Should Be Working With This Side-By-Side Refrigerator With Water Dispenser gefriertruhe mit ca 300 liter nutzinhalt testsieger 2025
See What Large U Shaped Sectional Tricks The Celebs Are Using Large U Shaped Sectional
10 Websites To Help You Be A Pro In Shipping Container Architecture Shipping Container Homes
See What Window Frame Seals Tricks The Celebs Are Making Use Of window Frame Seals
What's The Job Market For Cheap MDMA Online Professionals? Cheap MDMA Online (Md.Entropia.De)
5 Buy A Motorcycle License Tips You Must Know About For 2024 FüHrerschein Kaufen FüR 500 Euro (Https://Git.Rpjosh.De/)
UPVC Front Door Repair Tools To Improve Your Daily Lifethe One UPVC Front Door Repair Trick That Everyone Should Learn upvc front door Repair [https://king-wifi.win]
10 Life Lessons That We Can Learn From Recliner Couches For Sale couch Uk
Find Out What Height-Adjustable Desk Table Tricks The Celebs Are Making Use Of Escritorio Con Escritorio Eléctrico De Altura Ajustable (socialinplace.com)
7 Helpful Tricks To Making The Most Out Of Your Citroen Berlingo Van Key Replacement citroen Berlingo key replacement [forum-directory.com]
Five Killer Quora Answers To Foggy Glass Replacement foggy glass Replacement
15 Reasons Not To Ignore Buy A Cheap Chest Freezer einbaukühlschrank no frost
Why Buy Portable Pressure Washer May Be Greater Dangerous Than You Think leichter hochdruckreiniger kaufen (chimeear57.werite.net)
10 Myths Your Boss Has Regarding Online Psychiatrist Cost of private psychiatrist, https://hack.Allmende.io/bYOmljIWT0OqR81PKgtRgA,
This Is The Complete Listing Of Glazier Near Me Dos And Don'ts local glazier; hedge.fachschaft.informatik.uni-Kl.de,
15 Gifts For That Mitsubishi Key Replacement Lover In Your Life Mitsubishi Key Replacement Near Me (posteezy.com)
Begin By Meeting The Steve Jobs Of The Door Jamb Seals Industry Adhesive Weather Stripping
The Ultimate Glossary Of Terms About Get Switzerland Driving License Schweizer FüHrerschein Erhalten
Nine Things That Your Parent Taught You About Emergency Board Up Company Emergency Board Up Company
9 Lessons Your Parents Teach You About Kia Replacement Key Uk Kia Replacement Key
10 Fundamentals To Know Robot Vacuum And Mop Self-Empty You Didn't Learn At School Self Cleaning Vacuum Robot
Guide To Jaguar Car Key: The Intermediate Guide The Steps To Jaguar Car Key Jaguar Car Key
10 Inspirational Graphics About Planing Machines Discounts holzbearbeitungshobelmaschinen online kaufen
5 Killer Quora Answers On Upvc Door Panel Renovation UPVC Door Panel Renovation
20 Important Questions To Be Asking About U-Shaped Sectional Sofa Before You Decide To Purchase It sectional couch with chaise lounge (https://clientsarah8.Werite.net/)
Why No One Cares About Triple Bunk Beds For Adults Triple Bunk Bed For Adults
It's The Ugly Real Truth Of Built-in 60 Cm Oven Offer backofen pyrolyse güNstig
The 10 Most Terrifying Things About Sash Window Services In My Area Sash Window Services In My Area
What's The Current Job Market For Accident Lawyer USA Professionals Like? Accident Lawyer USA; funsilo.date,
A An Instructional Guide To Cordless Hot Glue Gun Reviews From Start To Finish Profi Werkzeug Online Bestellen
10 Tell-Tale Warning Signs You Need To Get A New Psychiatric Evaluation private Psychiatrist cost uk
This Week's Top Stories About Tumble Dryers For Home Tumble Dryers For Home wäschetrockner im Angebot Kaufen
Need Inspiration? Look Up De Longhi Coffee de'longhi Coffee
10-Pinterest Accounts You Should Follow Ford Car Key Ford Car Key Replacement Cost (https://articlescad.com/30-inspirational-quotes-on-replacement-key-for-ford-focus-287879.html)
9 . What Your Parents Taught You About ADHD In Adults Test adhd In adults test
What's The Job Market For Professional Accident Lawyer Professionals? Professional accident Lawyer
Five Killer Quora Answers On Hyundai Amica Replacement Key hyundai Amica replacement key
The 10 Most Scariest Things About Interior Lighting UK interior Lighting
You'll Never Guess This Dehlonghi Coffee Machine's Tricks dehlonghi coffee Machine
What's The Job Market For Stable 3 Wheel Scooter Professionals? Stable 3 Wheel Scooter (hedge.fachschaft.informatik.uni-kl.de)
Why Do So Many People Want To Know About Triple Bed Bunk? Triple Bunk Bed With Mattress Included
What's The Job Market For Volvo Spare Key Professionals Like? Volvo Spare Key
20 Things That Only The Most Devoted Durable Impact Wrench Fans Understand Schlagschrauber-Bewertungen
Find Out What Swift Cat Flap Installation Tricks The Celebs Are Utilizing cat flap with lock installation
See What Nexpresso Coffee Maker Tricks The Celebs Are Using Nexpresso Coffee Maker (Hedge.Fachschaft.Informatik.Uni-Kl.De)
The 10 Most Terrifying Things About Conservatory Frame Restoration Conservatory Frame Restoration
What's The Current Job Market For Baby Cribs That Turn Into Beds Professionals Like? Cribs That Turn Into Beds
15 Best Ovens On Sales Bloggers You Must Follow Best Ovens
A How-To Guide For Buy Milling Machines For Schools From Beginning To End Gebrauchte FräSmaschinen Kaufen
Auto Accident Injury Lawyer Techniques To Simplify Your Daily Lifethe One Auto Accident Injury Lawyer Trick That Every Person Should Be Able To Auto Accident Injury Lawyer
Table Drill Explained In Less Than 140 Characters Akkubohrmaschine Test (beluna-versand-De77045.mybuzzblog.com)
How The 10 Worst Instant Belgium Driver's License Mistakes Of All Time Could Have Been Prevented Betaalbaar Belgisch Rijbewijs
The Best Norwegian Driver's License For Sale Tricks To Transform Your Life Norsk FøRerkort Til Salgs
Local Glazier Tools To Ease Your Everyday Lifethe Only Local Glazier Technique Every Person Needs To Learn Local Glazier
Five Tools That Everyone Is In The Electric Oven & Hob Industry Should Be Making Use Of Electric Ovens and hobs
What's The Job Market For Professional House Locksmith Professionals? Professional House Locksmith (Forum.Finveo.World)
Learn About Electric Fireplace Heater Wall Mount While Working From The Comfort Of Your Home Wall-Mounted Electric Fireplace
The Best Way To Explain Bedside Bassinet To Your Mom Baby Bedside Sleeper
9 . What Your Parents Taught You About Accident Insurance Claim Lawyer Accident Insurance Claim Lawyer
10 Things That Your Family Taught You About House Key Cutting House Key Cutting
Nine Things That Your Parent Teach You About Cordless Wood Saw Cordless Wood Saw
What Is The Reason Door Handle Fix Is The Best Choice For You? door handle Replacement
See What Auto Accident Injury Lawyer Tricks The Celebs Are Utilizing Auto Accident Injury Lawyer
You'll Never Be Able To Figure Out This Buy Industrial Lighting UK's Benefits industrial lighting
The 10 Most Scariest Things About All Terrain Stroller all Terrain Stroller
Five Killer Quora Answers On Maintenance For Conservatory maintenance for conservatory
11 "Faux Pas" That Are Actually Okay To Make With Your Tools Online tool Shop (Https://postheaven.net/)
12 Guttering Professionals Facts To Make You Think Twice About The Cooler. Cooler Gutter Replacement
Guide To Online Co Codamol Prescription: The Intermediate Guide Towards Online Co Codamol Prescription Online co codamol Prescription
20 Up And Coming Pressure Washer For Patio Stars To Watch The Pressure Washer For Patio Industry Haaga 477 Profiline Preis
Why You Should Focus On Improving Chisel Hammer With Hex Shank Stemmhammer 50 Joule Preis
See What Secure Window Handle Replacement Tricks The Celebs Are Using Secure Window Handle Replacement
The 10 Most Terrifying Things About Lexus Replacement Key Lexus Replacement Key
Don't Buy Into These "Trends" Concerning Baby Cot cheap Baby cots for sale
5 Killer Quora Answers To Window Hinge Replacement Window Hinge Replacement
10 Things We All Hate About Baby Cots Travelcot
5 Laws That Will Help The Double Glazing Upgrade Industry glass Installation
Ten Reasons To Hate People Who Can't Be Disproved Best Cot Bed Best infant cribs
See What Skoda Octavia Replacement Key Cost Tricks The Celebs Are Utilizing Skoda Octavia Replacement Key
What's The Current Job Market For Continental WinterContact TS 870 Professionals? Continental Wintercontact ts 870
10 Things That Your Family Teach You About Accident Law Firm USA Accident Law Firm Usa
20 Trailblazers Setting The Standard In Ergonomic Desks Online Escritorios EléCtricos De Altura Ajustable
See What Buy Amitriptyline No Rx Tricks The Celebs Are Utilizing Buy Amitriptyline No Rx (scientific-programs.science)
Five Killer Quora Answers To Emergency Window Hinge Repairs Emergency Window Hinge Repairs
3 Ways The Couches Online Influences Your Life Comfortable affordable couches
Effective Weight Loss Drugs Online Tools To Help You Manage Your Daily Lifethe One Effective Weight Loss Drugs Online Trick That Should Be Used By Everyone Know Effective Weight Loss Drugs Online - wavesocialmedia.com -
What's The Job Market For Citroen Replacement Key Fob Professionals Like? citroen replacement key Fob
See What Double Glazed Window Repairs Tricks The Celebs Are Making Use Of Double Glazed Window Repairs
Private ADHD Assessment Tools To Improve Your Day-To-Day Life private adhd assessment adults
The Next Big Thing In The ADHD Assessment UK Industry private adhd diagnosis Glasgow (rant.li)
20 Things That Only The Most Devoted Couch L Shape Fans Should Know L Shaped Sectional Sofas
What Is ADHD Assessment Adults And Why You Should Take A Look private Adhd assessment bedfordshire
15 Reasons Not To Ignore UPVC Door Specialist UPVC Door Specialists
The Best Norwegian Drivers License Purchase Tricks To Transform Your Life Selger Av Norsk FøRerkort
The 10 Scariest Things About Porsche Panamera Key Replacement Cost porsche panamera key replacement cost
Why Best Height-Adjustable Desk Tables Is Still Relevant In 2024 Compra Mesa De Altura Ajustable Online
The 10 Most Terrifying Things About Window Hinge Repair Techniques Window Hinge Repair Techniques
15 Things You've Never Known About Wine Fridge Price Small Wine Cooler
Pirelli Tires Online Tools To Help You Manage Your Daily Life Pirelli Tires Online Trick Every Individual Should Be Able To Pirelli Tires Online
The Benefits Of Apply For A2 Driver's License Digitally At Least Once In Your Lifetime Führerschein Digital kaufen
5 Killer Quora Answers To Samsung QLED TV Deal Samsung QLED TV Deal
10 Apps To Aid You Control Your Best Fridge Online Waschmaschine 8Kg Test
5 Laws That Can Help Those In Mitochondrial Health Supplements Industry Mitolyn Official Website Buy
You'll Never Be Able To Figure Out This Sash Window Refurbishment Cost's Benefits Sash Window Refurbishment Cost
See What Door Lock Replacement Service Tricks The Celebs Are Using door lock replacement service
You'll Never Guess This Window Weather Stripping's Tricks Window Weather Stripping
All Terrain Travel System: A Simple Definition Best All Terrain Travel System (https://hedge.fachschaft.informatik.uni-kl.de/s/sfO8Bk2Ah)
15 Tilt And Turn Windows Bloggers You Should Follow Fix Tilt And Turn Windows
12 Companies Are Leading The Way In Apply For Danish Driver's License Få Et Kørekort I Danmark (masjidwasl.com)
15 Unquestionably Good Reasons To Be Loving Buy A Cheap Freestanding Hob Backofen Set Mit Kochfeld Kaufen
What's The Current Job Market For Double Glazing Leak Repair Professionals Like? Double Glazing Leak Repair
See What Mitsubishi Keys Replacement Tricks The Celebs Are Using Mitsubishi Keys Replacement
9 Lessons Your Parents Taught You About Reliable Door Handle Repair Door Handle Repair
Guide To ADHD Private Assessment UK: The Intermediate Guide On ADHD Private Assessment UK ADHD Private Assessment UK
Guide To Mazda Replacement Key Cost: The Intermediate Guide In Mazda Replacement Key Cost mazda replacement key cost
The Reasons Why Adding A Box Freezers To Your Life Will Make All The Difference Deep Freezers
20 Best Tweets Of All Time About Private ADHD Assessment Glasgow Private Adhd Assessments In Glasgow
10 Meetups On Ovens Built In You Should Attend Integrated Ovens Uk
Guide To Best 305mm Mitre Saw: The Intermediate Guide The Steps To Best 305mm Mitre Saw Best 305mm mitre saw
8 Tips To Improve Your Psychiatrists Near Me Game private online Psychiatrist
15 Best Door Locks Replacement Bloggers You Must Follow Best Door Locks Replacement (Everest.Ooo)
9 Lessons Your Parents Taught You About American Fridge Freezers For Sale American Fridge Freezers For Sale
What Is It That Makes Pull Out Sofa So Popular? pull out Sofa bed
Guide To Stylish 3 Wheel Scooter: The Intermediate Guide For Stylish 3 Wheel Scooter Stylish 3 Wheel Scooter
This Is The Intermediate Guide Towards Cotbed Baby Cotbed
The 9 Things Your Parents Taught You About Key Fob Mini Cooper Key Fob Mini Cooper
15 Reasons Why You Shouldn't Ignore Motorised Treadmill power
The Top Reasons For Comfy Couch's Biggest "Myths" About Comfy Couch Could Actually Be Accurate black couches
3 Reasons The Reasons For Your Private ADHD Diagnosis Near Me Is Broken (And How To Repair It) private Psychiatry near Me
See What Bedside Cot Beds Tricks The Celebs Are Using Bedside Cot Beds
See What Top-Rated Tilt And Turn Window Repair Service Tricks The Celebs Are Utilizing Top-Rated Tilt And Turn Window Repair Service
You'll Never Be Able To Figure Out This Pull Out Sleeper Couch's Secrets Pull Out Sleeper Couch
5 Tools That Everyone In The Michelin Winter Tire Prices Industry Should Be Utilizing goodyear ganzjahresreifen erfahrungen
Where Is Expert Double Glazing Repair Be One Year From What Is Happening Now? Double Glazing Repairs (http://volleypedia-org.50and3.com/index.Php?qa=user&qa_1=textcrab0)
10 Tips To Know About Double Pram side By Side double pram
Accident Injury Compensation Claim Lawyer Tools To Ease Your Daily Life Accident Injury Compensation Claim Lawyer Trick That Everybody Should Know Accident Injury Compensation Claim Lawyer
5 Laws Everyone Working In Baby Cribs For Sale Should Know best travel cots uk
5 Killer Quora Answers On Coffee Beans 1kg UK Coffee Beans 1Kg Uk
Unexpected Business Strategies Helped Built In Electric Oven To Succeed Built-in Oven and hob
9 Lessons Your Parents Teach You About Robot Vacuum Robotic Vacuum Cleaner On Sale
The Best Manual Treadmill For Home Tricks To Make A Difference In Your Life Best Manual Treadmill
What's The Job Market For Wooden Baby Bed Professionals? Wooden Baby Bed
You'll Never Guess This Delonghi Coffee Machine With Grinder's Tricks Delonghi Coffee Machine With Grinder
See What Automatic Folding Electric Wheelchair UK Tricks The Celebs Are Using Automatic Folding Electric Wheelchair UK
Why Metal Grinder Isn't As Easy As You Imagine Trockenbauschleifer Preis
You'll Be Unable To Guess Accident Law Firm USA's Tricks Accident Law Firm USA
Expert Advice On CNC Milling Machine For Metal From A Five-Year-Old Werkzeugmaschinen Online Shop
The 10 Most Terrifying Things About Accident Claim Lawyer Accident Claim Lawyer
The 10 Most Terrifying Things About Tilt And Turn Window Restoration Tilt And Turn Window Restoration
What's The Job Market For Honda Jazz Replacement Key Professionals? Honda Jazz Replacement Key
Honda Lost Key Replacement Tools To Streamline Your Daily Lifethe One Honda Lost Key Replacement Trick That Every Person Must Know Honda Lost Key Replacement
8 Tips To Improve Your Injury Lawsuit Lawyer Game Accident Injury Lawsuit Lawyer
Guide To Mini Cooper Replacement Key Cost UK: The Intermediate Guide The Steps To Mini Cooper Replacement Key Cost UK mini cooper replacement key Cost
Kia Replacement Key Price Uk Tips To Relax Your Daily Life Kia Replacement Key Price Uk Trick That Should Be Used By Everyone Know Kia Replacement Key Price Uk
Why You Should Focus On Enhancing 6ft Shipping Container 6ft shipping Containers
What's The Current Job Market For Best Sash Window Repair Contractors Professionals Like? Best Sash Window Repair Contractors
You'll Never Be Able To Figure Out This Accident Law Firm USA's Tricks Accident Law Firm USA
See What Local Window Doctor Tricks The Celebs Are Making Use Of Local Window Doctor
The Most Effective Reasons For People To Succeed At The Affordable Couches Industry Most Comfortable sofa
Guide To 20ft Shipping Container New: The Intermediate Guide Towards 20ft Shipping Container New 20ft Shipping Container New
10 Untrue Answers To Common Diy Window Hinge Repair Questions Do You Know The Correct Answers? Window Hinge Problems
How To Explain Fridge UK To Your Grandparents Waschmaschine mit trockner funktion vergleich
Guttering Solutions Tools To Help You Manage Your Everyday Lifethe Only Guttering Solutions Trick Every Person Should Be Able To guttering Solutions
Guide To Local Accident Attorney: The Intermediate Guide For Local Accident Attorney Local accident attorney
What's The Job Market For Audi Replacement Key Service Near Me Professionals Like? audi replacement key service near me; legit-directory.com,
14 Cartoons About Fridges That'll Brighten Your Day Kondenstrockner angebot
15 Gifts For The Window Doctor Near Me Lover In Your Life Window Caulking [https://www.Celticsblog.Com]
The Biggest Issue With Volvo Key Replacement And What You Can Do To Fix It Volvo Key Replacement Near Me
What's The Job Market For How To Find A Lost Porsche Key Professionals? how to Find a lost porsche key
See What Kia Key Replacement Tricks The Celebs Are Making Use Of Kia Key Replacement
You'll Never Guess This Skoda Duplicate Key's Benefits Skoda Duplicate Key (Https://nephila.org/)
Guide To Folding Running Machine: The Intermediate Guide The Steps To Folding Running Machine Folding Running machine
A Guide To Couches From Start To Finish leather Couch uk (https://Rehabsteve.com/)
10 Best Books On Spanish Driving License distribuidor de permisos de conducir españoles
Swiss Driving Authority Tools To Make Your Everyday Life Schweizer FüHrerschein Erwerben
You'll Be Unable To Guess Couch With Pull Out Bed And Storage's Tricks couch with pull out bed and storage
5 Things Everyone Gets Wrong In Regards To Patio Door Repairs Near Me affordable patio Door repairs
See What Compact Bean To Cup Coffee Machine Tricks The Celebs Are Making Use Of Compact bean to cup coffee machine (output.jsbin.com)
What's The Job Market For Wooden Shipping Pallets Professionals Like? Wooden Shipping Pallets
How To Explain ADHD Specialist Near Me To A 5-Year-Old psychiatrist near Me Private Practice
5 Laws That Will Help To Improve The Benq W1800 Digital Projector Industry panasonic beamer zubehör
Why Is Window Repair Service So Popular? professional window repair
Five Killer Quora Answers To Coffee 1kg Beans Coffee 1Kg
The 10 Scariest Things About Wooden Pallets Vendor Wooden Pallets vendor
Bedside Cot For Safe Infant Sleep Tools To Ease Your Daily Lifethe One Bedside Cot For Safe Infant Sleep Trick That Every Person Must Learn Convertible Crib With Drawers
Guide To Folding Treadmill With Incline Uk: The Intermediate Guide On Folding Treadmill With Incline Uk folding treadmill with incline uk
See What Auto Accident Injury Lawyer Tricks The Celebs Are Making Use Of Auto Accident Injury Lawyer
What's The Job Market For Sash Window Maintenance Services Professionals? Sash Window Maintenance Services
The Top Double Decker Bed Adult Experts Have Been Doing 3 Things Adult Metal Bunk Beds
See What 1kg Coffee Beans Price UK Tricks The Celebs Are Using 1kg coffee beans price uk
15 Things You're Not Sure Of About High Quality Tumble Dryers Neueste Wäschetrockner
Five Killer Quora Answers To Mini Cooper Car Key Mini Cooper Car Key (Schoolido.Lu)
The 10 Most Scariest Things About Band Saw With Stand Band Saw With Stand
You'll Never Guess This Accident Injury Case Lawyer's Tricks Accident Injury Case Lawyer (https://Pattern-wiki.win/)
What's The Current Job Market For Intergrated Kitchen Professionals Like? intergrated Kitchen (funsilo.date)
You'll Never Guess This Sofa Bed Pull Out's Secrets Bed Pull Out (https://telegra.ph/A-Provocative-Remark-About-Pullout-Beds-10-15)
The Hidden Secrets Of Bedside Cot For First-Time Parents Cot With Drawers
15 Terms Everyone Involved In French Door Repair Services Industry Should Know French Door Repair Services In
Five Killer Quora Answers To Chest Freezer Frost Free Chest Freezer Frost Free
A Productive Rant About MItolyn Mitolyn Order
9 Things Your Parents Teach You About Replacement Parts For Window Handle Replacement Parts For Window Handle
9 Lessons Your Parents Teach You About Dewalt Power Tools For Sale Dewalt Power Tool
You'll Never Guess This Electric Wall Heater Fireplace's Tricks Electric Wall Heater Fireplace
What's The Job Market For Bedside Crib For Attachment Parenting Professionals Like? Bedside crib for Attachment parenting
10 Things That Your Family Taught You About Tilt And Turn Window Maintenance tilt And turn window maintenance
Solutions To Problems With Best No-Frost Fridge-Freezer Combination freistehende kühl-Gefrier-kombination no frost edelstahl kaufen - md.un-hack-bar.de -
Cotbeds: What's No One Is Talking About Top Rated Cots
What Is Self Emptying Robot Vacuums? History Of Self Emptying Robot Vacuums What Is Self Emptying Robot Vacuum
10 Reasons You'll Need To Be Aware Of Induction Hob Comparison Induktionskochfeld 80 Cm Autark Mit Rahmen GüNstig Kaufen
You'll Never Be Able To Figure Out This ADHD Test Online Adults's Tricks ADHD Test Online Adults
It Is Also A Guide To Buy A Fridge-Freezer Combination In 2024 Kühlschrank Mit 0 Grad Zone Test
Freezers For Sale 101 This Is The Ultimate Guide For Beginners Unterbaufähige Waschmaschine Kaufen
12 Companies Leading The Way In Washer Dryer Combo Offers waschtrockner-sets im abverkauf
See What Authentic Counterfeit Money Tricks The Celebs Are Utilizing Authentic Counterfeit Money
What's The Current Job Market For Cost Of Window Handle Replacement Professionals Like? cost of Window Handle replacement
What's The Job Market For Full Mental Health Assessment Online Professionals? Full Mental Health Assessment Online
See What Door Lock Replacement Service Tricks The Celebs Are Using door lock replacement service (https://mymatch.sundaytimes.lk/members/lycraghana5/activity/227813)
15 Things You've Never Known About Purchase Belgium Driving License Goedkoop Belgisch Rijbewijs
9 . What Your Parents Taught You About Car Key Smart Car Key Smart
The 9 Things Your Parents Teach You About Hyundai Tucson Key Replacement Cost Hyundai Tucson Key Replacement Cost
12 Companies Leading The Way In BMW Spare Key bmw Spare key replacement
11 Ways To Completely Redesign Your Glazier emergency Glass Repair
You'll Be Unable To Guess Range Rover Replacement Key Cost's Tricks Range Rover Replacement Key Cost (https://imoodle.win)
5 Killer Quora Answers On Tilt And Turn Window Crank Repair Tilt And Turn Window Crank Repair
Five Killer Quora Answers On Broken Window Repair Broken Window Repair
15 Best Twitter Accounts To Discover More About Online Psychiatrist private online psychiatrist
The Most Common Electric Wall Fireplace Heater Mistake Every Beginning Electric Wall Fireplace Heater User Makes Best Wall Mount Fireplace
Guide To Adult ADHD Assessment Private: The Intermediate Guide For Adult ADHD Assessment Private adult adhd Assessment private
15 Hot Trends Coming Soon About Buy Real Italian Driving License Patente Di Guida Online In Italia
What Window Hinge Repair Experts Experts Would Like You To Be Educated Repair Old Window Hinges
You'll Never Guess This Circular Saw Battery's Benefits circular saw battery [vittrup-oliver-2.hubstack.net]
Guide To Upvc Panel Experts: The Intermediate Guide The Steps To Upvc Panel Experts UPVC Panel Experts
The Best Advice You Could Ever Receive On 10 Bar Air Compressor ÖLfreier Kompressor Preisvergleich
5 Killer Quora Answers On Personal Injury Attorney Personal Injury Attorney
20 Reasons To Believe Buy A Fridge Will Never Be Forgotten Fridge Online
5 Laws Anyone Working In Tilt And Turn Window Hinge Adjustment Should Be Aware Of Tilt And Turn Windows
10 Top Facebook Pages Of All Time Concerning Volvo Car Key Volvo Car Keys
Built-In Cookers It's Not As Hard As You Think built in ovens electric - fancypad.Techinc.nl -
You'll Never Guess This Delonghi Coffee Machine Automatic's Tricks Delonghi Coffee Machine Automatic
10 Fundamentals Concerning House Locksmith You Didn't Learn At School House Locksmith Cost
20 Things That Only The Most Devoted Glass Repair Fans Know Double Glazing Condensation
What's The Current Job Market For Condensation In Windows Professionals? Condensation In Windows
See What Skoda Key Fob Tricks The Celebs Are Utilizing skoda key; Bestbizportal.com,
A Look Into Buy Language Certificate's Secrets Of Buy Language Certificate telc b1 prüFung certificate
The Little Known Benefits Of Car Ignition car ignition lock (pad.karuka.Tech)
You'll Never Guess This Lightweight Double Pushchair's Tricks Lightweight Double Pushchair
Volvo Replacement Key Cost Tools To Improve Your Daily Lifethe One Volvo Replacement Key Cost Technique Every Person Needs To Learn Volvo Replacement Key Cost
Home Robot Vacuum Isn't As Tough As You Think Vacuum Deals
See What How To Get A New Vauxhall Car Key Tricks The Celebs Are Making Use Of How To Get A New Vauxhall Car Key
ÖSD Certificate: 10 Things I Wish I'd Known Earlier ÖSD Prüfungen
15 Top Twitter Accounts To Learn More About House Locksmith Solutions residential Locksmith
See What Best Mitre Saws Tricks The Celebs Are Using Best Mitre Saws
Guide To Ramps For Mobility Scooters: The Intermediate Guide To Ramps For Mobility Scooters Ramps For Mobility Scooters
13 Things You Should Know About Ovens & Hobs That You Might Not Know Culinary tools
9 Things Your Parents Taught You About ADHD Test Online For Adults ADHD Test Online For Adults (https://lovewiki.Faith)
What's The Job Market For Exquisite Handmade Sofa Professionals? exquisite Handmade Sofa
9 Lessons Your Parents Taught You About Adult Bunk Beds UK adult Bunk Beds uk
You'll Never Be Able To Figure Out This Conservatory Frame Repair's Tricks conservatory frame repair (https://Forestrecess85.bravejournal.net/five-people-you-should-know-in-the-conservatory-frame-restoration-industry)
The Little Known Benefits Of Battery Circular Saw Battery Circular Saws (www.tomahawknation.com)
10 Myths Your Boss Is Spreading Concerning Large Chest Freezer Large Chest Freezer For Sale
10 Tell-Tale Symptoms You Need To Get A New Czech Driving License Guide ŘidičSké PřEdpisy V České Republice (clashofcryptos.trade)
15 Terms That Everyone Is In The French Door Repair Services Industry Should Know French Door Repair Services In
A Vibrant Rant About Robotic Mop Robot Vacuum
From Around The Web Here Are 20 Amazing Infographics About Mobility Scooter To Buy Near Me durable Mobility Scooters
Nine Things That Your Parent Teach You About Espresso Machine Under £500 espresso Machine Under £500
The 10 Most Scariest Things About Replacement Key For Vauxhall Meriva replacement key For vauxhall meriva
20 Reasons Why Bunk Beds In Sale Will Not Be Forgotten bunk Beds on sale
The 10 Most Scariest Things About Foggy Window Fix Foggy Window Fix
Guide To Land Rover Discovery 3 Replacement Key: The Intermediate Guide The Steps To Land Rover Discovery 3 Replacement Key land rover discovery 3 replacement key
Guide To UK Private Psychiatrist: The Intermediate Guide In UK Private Psychiatrist Uk private Psychiatrist
See What Seat Arosa Key Replacement Tricks The Celebs Are Using Seat Arosa key replacement
9 Things Your Parents Teach You About Free ADHD Test Online ADHD Test Online
What The Heck What Is Replacement Subaru Keys? Lost Subaru Key (https://hackmd.Okfn.de)
Guide To Jaguar Car Key: The Intermediate Guide In Jaguar Car Key Jaguar Car Key
You'll Never Guess This Patio Door Lock Repair's Tricks Patio Door Lock Repair
The 10 Most Terrifying Things About Sash Window Renovation Quotes Sash Window Renovation Quotes; fsquan8.cn,
Guide To Buy Cordless Workshop Essentials: The Intermediate Guide To Buy Cordless Workshop Essentials Cordless Workshop Essentials
How To Outsmart Your Boss On Door Hinge Replacement expert door hinge Repairman
The 10 Scariest Things About Seat Ibiza Replacement Key Seat Ibiza replacement key
15 Reasons To Not Ignore Bosch GHP 5-75 X Professional Nilfisk Hochdruckreiniger (Output.Jsbin.Com)
Five Killer Quora Answers On Mercedes Replacement Key Cost UK Mercedes Replacement Key Cost UK
The 10 Scariest Things About Accident Injury Lawsuit Lawyer Accident Injury Lawsuit Lawyer
The Intermediate Guide To Buying A Drivers License In Austria Österreichischer FüHrerscheinanbieter Online
9 Things Your Parents Teach You About MDMA Online Consultation MDMA Online Consultation
Getting Tired Of Bulk Coffee Beans? 10 Inspirational Sources That Will Invigorate Your Love coffee beans in bulk
From The Web: 20 Fabulous Infographics About Mental Health Assessments private psychiatrist Prices
Ten Vw Replacement Keys That Really Make Your Life Better vw replacement Keys
Guide To Mazda Car Key: The Intermediate Guide On Mazda Car Key Mazda Car Key
What Experts From The Field Of Pull Out Sofa Want You To Learn pull out sofa Beds - https://abci.info/,
The Reasons To Work On This Couches L Shaped L-Shaped Sectional
20 Things That Only The Most Devoted Cheap Belgian Driver's License Fans Should Know europees rijbewijs belgië, jobpile.uk,
Five Killer Quora Answers To Window Sealing Window Sealing
What's The Job Market For House Security Locksmith Professionals? House Security Locksmith
The Ultimate Guide To Driving License Validity comprar carteira de motorista (md.ctdo.de)
Five Killer Quora Answers To Order Goethe B1 Online Order Goethe B1 Online
Five Killer Quora Answers On UPVC Door Replacement Upvc Door Replacement
The 10 Most Scariest Things About Private Mental Health Diagnosis UK Private Mental Health Diagnosis UK
The Top Companies Not To Be In The Small Washer Dryer Industry waschtrockner-kombigeräTe kaufen
15 Shocking Facts About Tumble Dryers For Apartments You've Never Heard Of gebrauchte wäschetrockner online kaufen - scientific-programs.science -
Five Killer Quora Answers To Foldable Electric Wheelchair UK foldable electric wheelchair Uk
The 10 Scariest Things About Misted Glass Repair Glass Repair
Guide To Emergency Board Up Contractors: The Intermediate Guide To Emergency Board Up Contractors Emergency Board Up Contractors - reeves-mercado-5.blogbright.net -
You'll Never Guess This Accident Case Attorney's Tricks Accident case attorney
Why Comfy Couch Is Everywhere This Year couch sale uk
Guide To Easy-To-Use Planing Machines: The Intermediate Guide For Easy-To-Use Planing Machines Easy-To-Use Planing Machines
See What Door Lock Repair Tricks The Celebs Are Making Use Of Door Lock Repair
9 Things Your Parents Teach You About Self Mental Health Assessment Self Mental Health Assessment
Five Killer Quora Answers To Electric Oven & Hob hob (www.thesoldiermedia.com)
20 Questions You Should Ask About Compact Electric Treadmills Before Buying It electric treadmill for home
10 Life Lessons We Can Learn From High Quality Tumble Dryers Elektrische WäSchetrockner
See What Childs Bed With Slide Tricks The Celebs Are Using Childs Bed With Slide
Ten Startups That Will Revolutionize The Cheap Baby Cot Industry For The Better Toddler Travel Cot
15 Interesting Facts About Bedside Crib For Babies You Didn't Know Cots With Drawers
You'll Be Unable To Guess Electric Wall Heater Fireplace's Tricks Electric Wall Heater Fireplace
10 Inspiring Images About Places To Buy Headphones Buying Headphones
9 Lessons Your Parents Teach You About French Door Repair Diy French Door Repair Diy
What's The Job Market For Self Emptying Robot Vacuum And Mop Professionals? self emptying robot vacuum and mop
The 10 Scariest Things About Restoring Conservatory Windows restoring conservatory windows
Ten Twin Pushchairs That Really Help You Live Better Twin Pushchairs
5 Coffee Makers Leçons From The Professionals coffee Machine for business
Bedside Cot For Safe Infant Sleep Tools To Help You Manage Your Everyday Lifethe Only Bedside Cot For Safe Infant Sleep Trick That Everyone Should Be Able To Bedside Cot For Safe Infant Sleep
10 Startups Set To Change The Aluminium Patio Door Repairs Industry For The Better Patio Door Hardware Repair
Triple Sleeper Bunk: The Good, The Bad, And The Ugly 3 Single Bunk Beds
The Next Big Event In The 18V Cordless Demolition Hammer Industry stemmhammer sechskantaufnahme (elearnportal.science)
5 Killer Quora Answers To Foggy Glass Repair Foggy Glass Repair
포항출장마사지는 지역 어디든 방문 가능한 포항출장안마 전문 서비스입니다. 집·호텔·오피스 포항출장 관리로 이동 부담 없이 편안하게 이용 가능하며, 24시간 상담과 예약으로 언제든지 힐링을 제공합니다.
Really clear web site , thanks for this post.
Really clear web site , thanks for this post.
Wow! This could be one particular of the most helpful blogs We’ve ever arrive across on this subject. Actually Great. I am also an expert in this topic so I can understand your hard work.
You really make it seem so easy with your presentation but I find this topic to be really something which I think I would never understand. It seems too complicated and very broad for me. I am looking forward for your next post, I will try to get the hang of it!
NEAR마사지는 출장마사지와 출장안마 원하는 시간과 장소로 직접 찾아가는 맞춤형 마사지 서비스입니다. 복잡한 이동 없이 프라이빗한 환경에서 체계적인 관리를 받을 수 있어 일상 속 피로 회복에 도움이 됩니다.
토닥이 여성전용마사지 는 매장으로 직접 방문할필요 없이 고객님이 계신곳으로 직접 방문하여 마사지 서비스를 제공하고 있습니다. 여성만을 위한 섬세한 마사지 프로그램과 후불제 결제로 안심하시고 이용할수 있습니다.
Really clear web site , thanks for this post.
Good day webmaster, commenters and everybody else !!! The site was absolutely awesome! Lots of great info and inspiration, both of which we all need!b Keep ‘em coming… all of you can like a great job with such Concepts… can’t tell you just how much I, for just one appreciate all you decide to do.
You got a very great website, Glad I discovered it through yahoo.
천안출장마사지는 고객이 원하는 시간과 장소에 전문 테라피스트가 직접 방문하여 체계적인 마사지 프로그램을 진행하는 출장형 전문 테라피 서비스입니다
I really want to thank you for yet another great informative post, I’m a loyal visitor to this blog and I can’t say how much valuable tips I’ve learned from reading your content. I really appreciate all the hard work you put into this great blog.
I really want to thank you for yet another great informative post, I’m a loyal visitor to this blog and I can’t say how much valuable tips I’ve learned from reading your content. I really appreciate all the hard work you put into this great blog.
I really want to thank you for yet another great informative post, I’m a loyal visitor to this blog and I can’t say how much valuable tips I’ve learned from reading your content. I really appreciate all the hard work you put into this great blog.
순천출장마사지 서비스는 순천광역시 전역에서 편안하게 전문 마사지를 받을 수 있는 출장 홈타이 서비스입니다. 고객님이 계신 곳으로 여성 전문 테라피스트가 직접 찾아
천안출장마사지 두정동, 성정동, 불당동 등 천안 어디든 신속하게 방문합니다. 내상 걱정 없는 100% 후불제와 정찰제로 운영되어 안심하고 이용하실 수 있습니다. 엄선된 20대 베테랑 관리사가 선보이는 최상의 스웨디시와 홈타이로 지친 몸과 마음을 녹여드립니다. 24시간 연중무휴, 지금 예약하세요!
인천출장마사지 - 인천 전역에 24시간 여성 전문 마사지사가 찾아가는 출장 안마 서비스! 아로마, 스포츠, 커플 마사지로 피로와 스트레스를 합리적 가격에 풀어보세요
I really want to thank you for yet another great informative post, I’m a loyal visitor to this blog and I can’t say how much valuable tips I’ve learned from reading your content. I really appreciate all the hard work you put into this great blog.
안양출장마사지의 차별화된 가치 · 안양 전 지역 출장 가능 · 전문 테라피스트의 손길 · 철저한 위생과 청결 관리 · 24시간 예약 가능, 빠른 출장 시스템. 고객
Some truly nice and useful info on this site, likewise I conceive the style holds excellent features.
청주출장마사지 이동해야 하는 번거러움을 없이 편안하게 마사지 받을수 있어 너무 좋았습니다.
Really clear web site , thanks for this post.
Really clear web site , thanks for this post.
평택출장마사지. 24시간 365일 운영되는 출장마사지 서비스로, 고객님이 스케줄에 맞춰 원하는 시간과 장소로 관리사가 직접 방문하여 마사지를 제공하고 있습니다.
Really clear web site , thanks for this post.
Premium Quality Shrooms Gummies, Edibles, Capsules & Psychedelic Tea.
This web page is often a walk-through for all of the info you wanted about this and didn’t know who need to. Glimpse here, and you’ll definitely discover it.
I looked into how 탑플레이어포커 머니상 is presented within structured data discussions. Many sources describe system behavior, data accuracy, and how records are managed responsibly. From a general viewpoint, 탑플레이어포커 머니상 is best interpreted through documented and neutral sources.
Sunwin từ lâu đã khẳng định vị thế là "Cổng game bài đại gia" số 1 tại thị trường Việt Nam. Thuộc tập đoàn Suncity Group uy tín, Sunwin mang đến một không gian giải trí đẳng cấp quốc tế với giao diện 3D sắc nét và âm thanh sống động. Tại đây, người chơi có thể trải nghiệm hàng loạt tựa game đình đám từ Tiến lên miền Nam, Phỏm, Mậu binh cho đến các sảnh Casino trực tuyến và Slot game nổ hũ cực lớn. Với hệ thống bảo mật tối tân và cơ chế nạp rút tiền minh bạch, nhanh chóng, Sunwin cam kết mang lại sự an toàn tuyệt đối cho mọi thành viên. Hãy tham gia Sunwin ngay hôm nay để khẳng định bản lĩnh và tận hưởng những đặc quyền dành riêng cho giới thượng lưu.
You can get useful information about massage here.
Thanks for sharing such a helpful guide on ok win. The way you explained the okwin login process is simple and easy to follow. It really helps users understand how to access their accounts safely. This kind of clear information builds trust and makes the ok win platform more approachable for beginners and regular users alike.
day could get any better. I got a free hot dog and come back to my car and keith sweat ‘nobody’ is playing on backspin.|AshleyMKenny|
i got pregnant a couple of months ago and right now i am choosing the right kind of maternity clothes that is comfortable-
I happen to be writing to make you be aware of of the fantastic encounter my friend’s princess encountered visiting yuor web blog. She learned so many issues, which include how it is like to have an amazing coaching mood to have many others very easily fully grasp specific complex subject matter. You undoubtedly did more than our expectations. Thanks for producing those powerful, trusted, informative as well as easy tips about the topic to Jane.
Hey there! I know this is kinda off topic but I was wondering if you knew where I could get a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having difficulty finding one? Thanks a lot!
I appreciate making to debate this, I’m boldy about this and then fancy looking into more on this process topic. If it turns out would-be, any time you achieve professionalism, could you thoughts and feelings modernizing your own site utilizing even further help and advice? This can be very a good choice for me personally.
Its such as you read my thoughts! You seem to know a lot approximately this, such as you wrote the guide in it or something. I feel that you just could do with a few percent to drive the message home a little bit, but other than that, that is excellent blog. A fantastic read. I will definitely be back.
Outstanding read, I just passed this onto a colleague who was doing a little investigation on that. And he really bought me lunch because I discovered it for him smile So let me rephrase that: Thanks for lunch!
It¡¦s really a nice and helpful piece of info. I am glad that you shared this useful information with us. Please keep us up to date like this. Thanks for sharing.
well, skin cancer incidence would be increasing because of the hole on the ozone layer~
A lot of thanks for all of your work on this site. Betty really loves setting aside time for internet research and it is simple to grasp why. Most people learn all concerning the dynamic manner you convey rewarding tips on the website and as well encourage participation from visitors about this point plus my princess is undoubtedly being taught a great deal. Enjoy the rest of the new year. You have been conducting a fabulous job.
As such, these findings might shed new light on chronic pain. Park said.
You can definitely see your enthusiasm in the work you write. The arena hopes for even more passionate writers such as you who are not afraid to mention how they believe. All the time follow your heart.
This Just In: LeBron James is dropped from Nike and Picked up by SKETCHERS… new LeBRon James Shape UPs on the way!|tonydavisthedj|
What i don’t understood is actually how you are not actually much more well-liked than you may be now. You’re very intelligent. You realize therefore considerably relating to this subject, produced me personally consider it from so many varied angles. Its like women and men aren’t fascinated unless it is one thing to do with Lady gaga! Your own stuffs excellent. Always maintain it up!
Hey, very interesting article. My aunt and I have recently been searching for extensive details on this subject sort of stuff for a short time, however we didn’t until now. Do you think you can create a few youtube video clips concerning this, I do believe your web blog could well be more in depth if you ever did. In any other case, oh well. I will be viewing on this website in the near future. Email me to maintain me up-to-date. granite countertops cleveland
i’m fond of using vending machines because you can instantly get a drink or a snack,
This is a interesting line of content, very nice article. Thanks for sharing this post, good way of bring this subject to discussion. Keep up the great work !
i was suffering from colitis a couple of months ago and believe me, the pain is horrible”
It’s nearly impossible to find knowledgeable men and women about this topic, but you appear to be what happens you are dealing with! Thanks
I saw something about that subject on TV last night. Great post.
Really clear web site , thanks for this post.
Today, taking into consideration the fast life style that everyone is having, credit cards get this amazing demand throughout the economy. Persons coming from every area are using the credit card and people who are not using the credit card have made up their minds to apply for even one. Thanks for sharing your ideas on credit cards.
There are many content in the marketplace around this particular, I think getting there reference might encounter decided to get this to place or even article truly informative. Practical aim phrase this post is harmful. Merely I must enunciate how a data supplied the following has been special, merely repair much more in close proximity to full, helping along with other previous info obtain recently been actually excellent. The actual items you’ll take pleasure in carressed let us discuss important, thus My partner and i definitely will place several of the info right here to construct this kind of really perfect for completely the particular newbie’s here. Thank you these records. In fact beneficial!
you might have an amazing blog right here! would you like to make some invite posts on my weblog?
When June arrives to the airport, a man named Roy (Tom Cruise) bumps into her.
Hi” i think that you should add captcha to your blog”
hello there and thank you for your info – I have definitely picked up anything new from right here. I did however expertise some technical points using this web site, since I experienced to reload the site a lot of times previous to I could get it to load properly. I had been wondering if your hosting is OK? Not that I’m complaining, but slow loading instances times will very frequently affect your placement in google and can damage your quality score if ads and marketing with Adwords. Well I am adding this RSS to my e-mail and could look out for a lot more of your respective intriguing content. Ensure that you update this again very soon..
I have been exploring for a bit for any high-quality articles or blog posts in this sort of house . Exploring in Yahoo I at last stumbled upon this website. Reading this information So i¡¦m satisfied to show that I have an incredibly good uncanny feeling I came upon exactly what I needed. I most for sure will make certain to do not forget this website and give it a look a continuing.
It is actually a nice and helpful piece of information. I am happy that you just shared this useful information with us. Please keep us up to date like this. Thanks for sharing. rentacarkosovo
Can I just now say that of a relief to get somebody who actually knows what theyre speaking about on the web. You actually realize how to bring an issue to light and produce it important. Workout . need to look at this and fully grasp this side on the story. I cant think youre no more common because you definitely contain the gift.
A person necessarily help to make critically posts I’d state. That is the first time I frequented your web page and to this point? I amazed with the analysis you made to create this actual submit incredible. Excellent process!
There couple of fascinating points in time here but I do not determine if every one of them center to heart. There exists some validity but I am going to take hold opinion until I explore it further. Very good post , thanks and that we want much more! Included with FeedBurner as well
very nice post, i surely enjoy this fabulous website, keep on it
Really clear web site , thanks for this post.
Really clear web site , thanks for this post.
Really clear web site , thanks for this post.
24시 후불제 해피 태국출장마사지. 선입금 없음 · 도착 후 결제 | 전국어디든 · 신속방문. 24시간 운영 연중무휴. 후불제마사지 도착 후 결제
Really clear web site , thanks for this post.
Simply wanna comment on few general things, The website design is perfect, the articles is rattling fantastic : D.
Stick drift is one of the most common issues with controllers. Use a stick drift test to verify that your joysticks are properly calibrated. If you notice drift, you may need to clean or repair the joystick mechanism.
평택출장마사지 예약금 없이 100% 후불제로 부담 없이 이용할 수 있는 평택출장안마 전문 업체입니다. 숙련된 테라피스트가 직접 방문하여 타이마사지, 아로마마사지 등을 제공합니다.
This key fact write is get many site visitors. How should you publicize it? Doing it offers a fantastic customized style during strategies. My partner and i possessing a little something truly and / or excessive provide home elevators is the most essential element.
A great content material as well as great layout. Your website deserves all of the positive feedback it’s been getting. I will be back soon for further quality contents.
Before changing the protocol, confirm your controls. Strong ELISA controls tell you whether the problem is chemistry, technique, or sample-related. A reasonable control set usually includes a blank well, a zero standard (matrix without analyte), a mid-range standard, and a positive control sample that you know should land in range. If your kit includes recommended controls, follow them first. For custom assays, build a simple, repeatable control panel and keep it consistent between runs.
This was an interesting read, especially the practical points.
I recently came across related information about 경산출장마사지 in another context.
This reflection stays with the reader.
I really want to thank you for yet another great informative post, I’m a loyal visitor to this blog and I can’t say how much valuable tips I’ve learned from reading your content. I really appreciate all the hard work you put into this great blog.
인천출장마사지 인천출장안마를 찾으신다면 이 사이트에서 찾으세요. 인천에 위치한 가장 저렴하고 인기있는 한국, 러시아, 일본 다양한 국적의 홈케어 홈타이를 위치
수원출장마사지 24시간 연중무휴 운영! 여성 전문 테라피스트가 수원 전 지역 어디든 찾아갑니다. 아로마마사지·스포츠마사지·타이마사지 출장안마 서비스를 합리적
인천출장마사지는 밖으로 이동 없이 집·호텔·오피스텔·펜션으로 관리사가 직접 방문하는 출장안마 서비스입니다. 서울 전 지역 이용 가능합니다
타임케어 광명출장홈타이 - 광명출장마사지와 광명출장안마 광명홈타이 서비스를 전국 어디서나 24시간 편하게! 전문 마사지사의 맞춤 홈케어로 피로를 빠르게 해소
Interesting perspective! Do you think 아산출장마사지 would complement the exercises you mentioned?
My spouse and I stumbled over here by a different web address and thought I might check things out. I like what I see so i am just following you. Look forward to checking out your web page again.
Hey man, .This was an excellent page for such a hard subject to talk about. I look forward to reading many more great posts like these. Thanks
High-performance servers located within the region significantly reduce latency for a local audience, which is a key factor for SEO. Choosing reliable web hosting in nigeria means focusing on providers that maintain high-speed connections and secure environments, giving you peace of mind that your data is protected by firewalls.
Hey man, .This was an excellent page for such a hard subject to talk about. I look forward to reading many more great posts like these. Thanks
My spouse and I stumbled over here by a different web address and thought I might check things out. I like what I see so i am just following you. Look forward to checking out your web page again.
키탐넷은 '키스타임넷'으로 불리던 국내 성인용 정보·광고 플랫폼의 별칭으로 알려져 있습니다. 본 글은 키탐넷 관련 기본 개념, 이용 시 개인정보 보호
부산출장마사지,부산출장안마,부산홈타이 24시간 후불제 마인드좋은 관리사 상시대기 후불제 운영중입니다 안심하고 이용하세요
Leave a Comment